Key Takeaways
Hello Heart Hero. We know navigating your heart health can feel overwhelming, especially when a prescription meant to help might be causing other issues. If you've ever felt a strange flutter and wondered if your medication was the trigger, you're in the right place and your concerns are valid. Many people feel dismissed or uncertain when discussing these things, and you're right to seek clear, straightforward answers for your own peace of mind.
This guide is built for you. We're going to talk openly and honestly about common medications that cause atrial fibrillation (AFib). The purpose isn't to create alarm but to empower you with knowledge. Understanding which drugs can affect your heart rhythm allows you to have more informed, confident conversations with your healthcare provider.
Think of this as your personal briefing. We'll provide a direct look at specific medications that can sometimes throw your heart off its beat. You'll learn what to watch for and how to approach the topic with your doctor, giving you the tools needed to be an active partner in your own care. Let’s get started.
1. Adenosine (Adenocard)
Adenosine is a unique and powerful medication, often used in hospital settings to diagnose and stop a specific type of fast heart rhythm called paroxysmal supraventricular tachycardia (PSVT). While it's a lifesaver for PSVT, it holds a paradoxical secret: it is one of the more well-known medications that cause atrial fibrillation, even if it's just for a few moments, in a number of people who receive it.
How Adenosine Can Trigger Atrial Fibrillation
Adenosine works by briefly blocking the electrical signals passing through the atrioventricular (AV) node, which is like the heart's central electrical relay station. This action effectively "reboots" the heart's electrical system, stopping the rapid-fire circuit of PSVT.
However, its effect is incredibly short-lived, lasting only a few seconds. This abrupt interruption and the body's natural "fight-or-flight" hormonal response can create a chaotic electrical environment in the heart's upper chambers (the atria). This temporary instability can, in turn, trigger a new, disorganized rhythm: atrial fibrillation.
This effect is usually very brief, but for someone already anxious about a racing heart, it can be an unsettling experience. It's important to remember that this is a known side effect and medical teams are fully prepared to manage it.
Practical Tips
If you are ever in a situation where adenosine is recommended, understanding the process can help ease your concerns.
- Expect a Strange Sensation: People often describe a brief feeling of chest pressure, flushing, or a sense of "impending doom" as the medication works. This is normal and passes within seconds.
- Continuous Monitoring is Standard: You will be connected to an ECG monitor the entire time, allowing the medical team to see your heart's rhythm change in real-time.
- Defibrillator on Standby: As a standard precaution for any procedure involving heart rhythm medications, a defibrillator will be in the room and ready, just in case.
The following infographic provides a quick reference to the key characteristics of adenosine that explain why it acts so quickly and can sometimes trigger AFib.
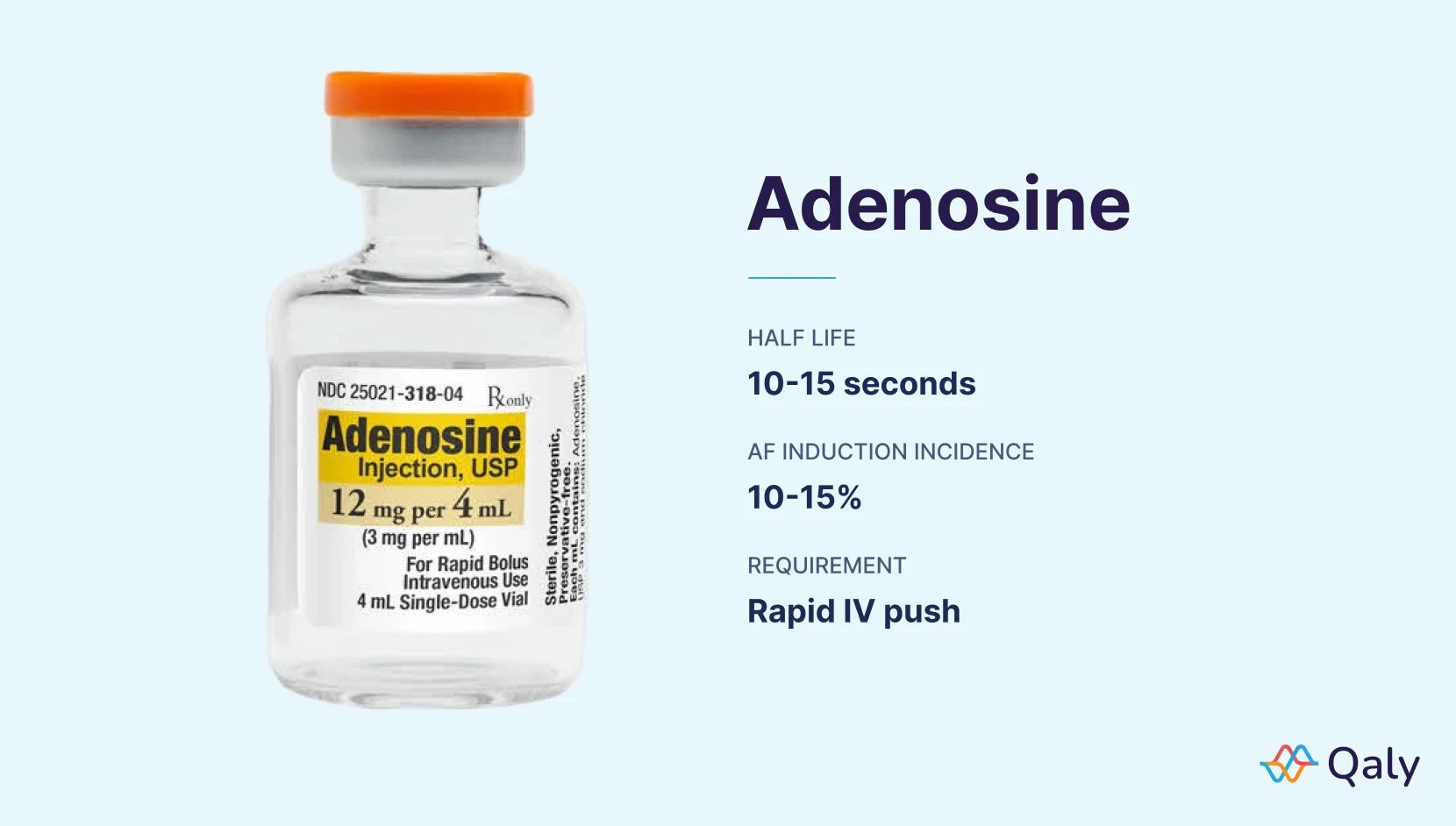
The data clearly shows why the drug's effects are so dramatic and short-lived, highlighting the potential for rhythm changes as the heart's systems quickly reset.
2. Digoxin (Lanoxin)
Digoxin is a long-standing medication derived from the foxglove plant, with a history stretching back to 1785. It's mainly used to help manage heart failure and to control the heart rate in people who already have atrial fibrillation. Despite its benefits, it carries a significant paradox: high levels of digoxin are a well-known cause of various heart rhythm problems, making it one of the classic medications that cause atrial fibrillation, particularly in certain at-risk individuals.
How Digoxin Can Trigger Atrial Fibrillation
Digoxin works by affecting a crucial enzyme in heart cells known as the sodium-potassium pump. This leads to an increase in calcium inside the cells, which strengthens the heart's contractions, a helpful effect for heart failure.
However, this is a delicate balance. When digoxin levels become too high (a condition called digoxin toxicity), the excess calcium can make the heart's upper chambers electrically unstable and irritable. This can cause them to fire off chaotically, overriding the heart's natural pacemaker and leading to the disorganized rhythm of atrial fibrillation. This risk is higher in the elderly and in those with poor kidney function, as the kidneys are responsible for clearing digoxin from the body.

Practical Tips
If your doctor prescribes digoxin, being proactive and aware can help you stay safe while benefiting from the medication. It's so important to watch for early signs of toxicity, as they can be subtle at first.
- Know the Early Warning Signs: Pay close attention to non-heart-related symptoms like nausea, vomiting, confusion, or visual changes (such as seeing yellow-green halos around objects). If you notice these, contact your doctor right away.
- Regular Blood Tests are Key: Your doctor will need to monitor the level of digoxin in your blood from time to time to ensure it's within the safe and effective range.
- Mind Your Kidneys and Electrolytes: Be sure your doctor knows about any kidney issues you have. Also, be cautious with medications like diuretics ("water pills"), which can lower your potassium levels and increase the risk of digoxin toxicity.
Understanding the potential symptoms of a heart arrhythmia can empower you to seek help sooner. Learn more about heart arrhythmia symptoms to stay informed and prepared.
3. Theophylline
Theophylline is a classic medication used to help people with breathing conditions like asthma and chronic obstructive pulmonary disease (COPD) breathe easier by relaxing the muscles around the airways. Despite its effectiveness, it carries a known risk and is a significant example of medications that cause atrial fibrillation, particularly at higher concentrations in the bloodstream.

How Theophylline Can Trigger Atrial Fibrillation
Theophylline's effect on the heart is directly related to its stimulating properties. It works by increasing the release of the body's natural stimulants, like adrenaline. This action can make heart muscle cells more "excitable" and prone to firing erratically.
This increased excitability creates an unstable electrical environment in the atria (the heart's upper chambers). When these chambers become overstimulated, they can lose their coordinated rhythm and slip into the chaotic, quivering state of AFib. This risk becomes much more pronounced when theophylline levels in the blood rise too high, a condition that can be surprisingly easy to reach as the drug has a narrow "safe" range.
Practical Tips
If you are prescribed theophylline, proactive management and open communication with your doctor are key to using it safely.
- Regular Blood Tests are Crucial: Theophylline has a narrow "safe" range. Your doctor will need to monitor the levels in your blood regularly to ensure the dose is effective but not high enough to cause dangerous side effects like AFib.
- Be Aware of Interacting Factors: Your age, liver function, and other medications can all affect how your body processes theophylline. Be sure your doctor knows your full medical history and all other drugs or supplements you take.
- Report Symptoms Immediately: If you experience palpitations, a racing heart, dizziness, or lightheadedness while on theophylline, contact your healthcare provider right away. It could be a sign that your dose needs adjustment.
- Consider Alternatives if at High Risk: If you have a pre-existing history of arrhythmias or other heart conditions, it's worth discussing alternative bronchodilators with your doctor. Newer medications may offer a safer profile for you.
4. Dobutamine (Dobutrex)
Dobutamine is a powerful intravenous medication used in critical care settings, like the ICU, to help a weakened heart pump more effectively. It's often given during serious events like acute heart failure. While it is a crucial tool for supporting heart function, it is also well-recognized as one of the medications that cause atrial fibrillation, with a number of patients developing the arrhythmia during treatment.
How Dobutamine Can Trigger Atrial Fibrillation
Dobutamine works by stimulating beta-1 receptors in the heart, which increases the heart's strength and rate. This direct stimulation, while helpful, can also make the heart's upper chambers more electrically irritable and prone to firing chaotically.
This effect is directly related to the dosage; higher infusion rates significantly increase the risk. As the medication boosts the heart's activity, it can overwhelm the normal electrical pathways, creating the perfect storm for disorganized signals to take over and start atrial fibrillation. This is a common occurrence during dobutamine stress tests, where the drug is intentionally used to stress the heart under controlled conditions.
Practical Tips
If you or a loved one are in a situation requiring dobutamine, it's typically a serious medical event. Understanding the monitoring process can provide some reassurance during a stressful time.
- Start Low, Go Slow: Medical teams will always begin the infusion at the lowest possible effective dose and increase it gradually while closely observing your heart's response.
- Constant ECG Monitoring is Mandatory: You will be connected to a continuous ECG monitor, allowing the healthcare team to instantly detect any rhythm changes like AFib.
- Antiarrhythmic Medications on Standby: Hospitals are well-prepared for this side effect. Medications to control heart rate or restore normal rhythm are kept readily available.
- Alternative Options Exist: If atrial fibrillation develops and becomes problematic, your doctors may consider switching to a different medication that has a lower risk of causing arrhythmias.
Dobutamine's mechanism of action, while life-saving for heart failure, highlights the delicate balance of your heart's electrical system. To understand more about how different heart medications can have complex side effects, you can learn more about the side effects of blood pressure medications and how they impact your body.
5. Levothyroxine (Synthroid, Levoxyl)
Levothyroxine is a very common medication for managing hypothyroidism (an underactive thyroid), restoring normal hormone levels and energy. However, finding the right dose is a delicate balance. While essential for your health, getting too much of this synthetic thyroid hormone can be one of the medications that cause atrial fibrillation, especially in older adults or those with pre-existing heart conditions.

How Levothyroxine Can Trigger Atrial Fibrillation
Levothyroxine works by mimicking your body's natural thyroid hormone, T4. When levels are too high, it essentially creates a state of hyperthyroidism, which puts the entire body into overdrive, including the heart.
This overstimulation can lead to AFib in a few ways. It increases the heart's overall workload, makes the heart muscle more sensitive to adrenaline, and can directly alter the electrical properties of cardiac cells. When your thyroid stimulating hormone (TSH) levels are pushed too low (a sign of too much thyroid medication), the risk of developing this chaotic heart rhythm goes up significantly. For a deeper understanding, you can learn more about the link between thyroid disorders and your heart.
Practical Tips
If you are prescribed levothyroxine, open communication with your doctor and awareness of your body are key to using it safely.
- Start Low, Go Slow: Especially in older patients or those with known heart issues, doctors often start with a very low dose and increase it gradually over several weeks or months.
- Consistent TSH Monitoring: Regular blood tests to check your TSH levels are crucial, particularly when starting or changing a dose, to ensure your levels are in the optimal range.
- Report New Symptoms: Be sure to tell your doctor immediately if you notice new symptoms like a racing heartbeat, palpitations, shakiness, or increased anxiety, as these can be signs that your dose is too high.
- Consider a Baseline Heart Check: If you have risk factors for heart disease, your doctor may recommend a baseline electrocardiogram (ECG) before you begin therapy to understand your heart's current state.
6. Albuterol (ProAir, Ventolin)
Albuterol is a life-saving rescue inhaler for millions of people with asthma and COPD, working quickly to open up airways during breathing difficulties. While it’s designed to target the lungs, its effects can sometimes spill over to the heart, making it one of the more common medications that cause atrial fibrillation, especially in certain situations.
How Albuterol Can Trigger Atrial Fibrillation
Albuterol works by stimulating beta-2 receptors in the muscles of the airways, causing them to relax. However, the heart also contains beta receptors. When higher doses of albuterol are used, or when it's used very frequently, the medication can start stimulating the heart's receptors as well.
This stimulation can increase your heart rate, make the heart contract more forcefully, and unfortunately, make the heart's electrical system more irritable. For individuals who are already susceptible due to age, pre-existing heart conditions, or low potassium levels, this extra electrical "noise" can be enough to disrupt the normal rhythm and kick off an episode of atrial fibrillation.
Practical Tips
If you rely on albuterol, managing its use wisely is key to protecting your heart. It’s a necessary medication, but understanding its potential effects empowers you to use it more safely.
- Use the Lowest Effective Dose: Always use the minimum number of puffs needed to relieve your symptoms. If you find yourself needing it more often than prescribed, it’s a sign that your underlying lung condition may need better control.
- Master Your Inhaler Technique: Using your inhaler correctly (with a spacer if recommended) helps ensure more of the medicine gets to your lungs and less is absorbed into your bloodstream where it can affect your heart.
- Monitor Your Heart Rate: Be aware of your heart's reaction after using albuterol, especially with nebulizer treatments. If you feel sustained, rapid, or irregular heartbeats, it's important to take note. You can learn more about when to see a doctor for heart palpitations for additional guidance.
- Discuss Your Cardiac History: Make sure your doctor knows about any heart conditions you have. They can help you weigh the risks and benefits of using albuterol.
7. Flecainide (Tambocor)
Flecainide is a powerful antiarrhythmic medication prescribed to maintain a normal heart rhythm and prevent certain types of arrhythmias, including atrial fibrillation. In a twist of irony, this very medication designed to control rhythm disturbances is also on the list of medications that cause atrial fibrillation or other serious arrhythmias under specific circumstances.

How Flecainide Can Trigger Atrial Fibrillation
Flecainide works by blocking sodium channels in the heart's muscle cells, which slows down the speed of electrical signals. This is meant to interrupt the chaotic circuits that cause rhythms like AFib. However, this same mechanism can be a double-edged sword.
In individuals with underlying structural heart disease, such as a history of a heart attack or heart failure, this slowing of conduction can become dangerous. It can create areas of uneven electrical activity, setting the stage for new, life-threatening arrhythmias to begin. The medication can also sometimes convert atrial fibrillation into a more organized but still rapid rhythm called atrial flutter, which can be challenging to manage.
Practical Tips
If your doctor is considering flecainide, they will take careful steps to ensure it is a safe option for you. Understanding these precautions can help you feel more confident in your treatment plan.
- Heart Health Check is Essential: Before starting, your doctor should order an echocardiogram (an ultrasound of your heart) and a baseline ECG. This is to confirm you do not have structural heart disease, which is a key safety requirement for using this drug.
- Start Low and Go Slow: Treatment typically begins with a low dose that is gradually increased. This allows your doctor to find the most effective dose with the lowest risk of side effects.
- Watch for ECG Changes: You will have follow-up ECGs to monitor for any significant changes. If a measurement called the QRS complex widens too much, it may be a sign the dose is too high.
- Know the "Pill-in-the-Pocket" Strategy: For some people with infrequent AFib episodes, doctors prescribe flecainide to be taken only as needed when an episode starts. Be sure you fully understand your doctor's instructions on when and how to use it this way.
Medications Causing Atrial Fibrillation: Comparison of 7 Agents
Your Next Step: Partnering With Your Doctor (And Your Data)
Navigating the world of heart health can feel like a lot, especially when you learn that a necessary treatment might also carry risks. Throughout this guide, we've looked at several common medications that cause atrial fibrillation as a potential side effect. The goal isn't to make you worried, but to make you aware. Recognizing that a medication could be a trigger is the first, most crucial step toward regaining control and feeling better.
The single most important takeaway is this: never stop or change a prescribed medication on your own. The conditions these drugs treat are serious, and the benefits often far outweigh the potential for heart rhythm disturbances. Instead, use this knowledge to have a more productive, collaborative conversation with your healthcare team.
Turning Information Into Action
So, what do you do with this new information? You transform it into a powerful tool for your next doctor's appointment. Instead of feeling anxious or uncertain, you can walk in prepared, confident, and ready to be an active partner in your own care.
Here’s a practical, step-by-step approach:
- Track Your Symptoms: Keep a simple log of when you feel palpitations, lightheadedness, or shortness of breath. Note the time of day and what you were doing. This context is incredibly valuable.
- Leverage Your Tech: If you use a wearable device like an Apple Watch, Fitbit, or a portable ECG monitor like Kardia, you have a data-gathering superpower in your pocket. Capture an ECG recording whenever you feel symptoms.
- Prepare Your Questions: Before your appointment, write down exactly what you want to discuss. Frame it collaboratively. For example, you could say, "I've been tracking my heart rhythm and noticed more frequent episodes of what feels like AFib since starting my new medication. I read this can sometimes be a factor. Could we look at my ECGs and discuss if my dosage is right for me?"
The Power of Concrete Data
This is where your personal data can truly change the dynamic of your healthcare. It's understandable to feel skeptical or unheard, and many people struggle to convey their experiences effectively. A subjective feeling is hard for a doctor to act on, but objective data is a different story.
Key Insight: A doctor can't see what you feel, but they can analyze what you record. Bringing ECGs from your home device to an appointment changes the conversation from "I feel funny sometimes" to "Here is a documented arrhythmic event that occurred at 3 PM yesterday."
This approach bridges the gap between your lived experience and your doctor's clinical expertise. It allows them to see precisely what's happening to your heart rhythm, making it easier to connect the dots between your symptoms and the potential medications that cause atrial fibrillation. This evidence-based approach validates your concerns and empowers your doctor to make the most informed decisions about your treatment plan. You are the leading expert on your body; combining that expertise with clear data is the fastest path to a healthy heart and lasting peace of mind.
Don't leave the interpretation of your heart data to chance. Get your ECGs from your Apple Watch, Fitbit, or Kardia device analyzed by certified cardiac technicians with Qaly. For less than the cost of a single co-pay, you can have expert-verified reports to share with your doctor and gain the clarity you deserve. Learn more about how Qaly can help you manage your heart health today.
On the Qaly app, human experts review your ECGs and explain how your treatment is affecting your heart. Start monitoring today.










.png)
.png)