Key Takeaways
Hello Heart Hero.
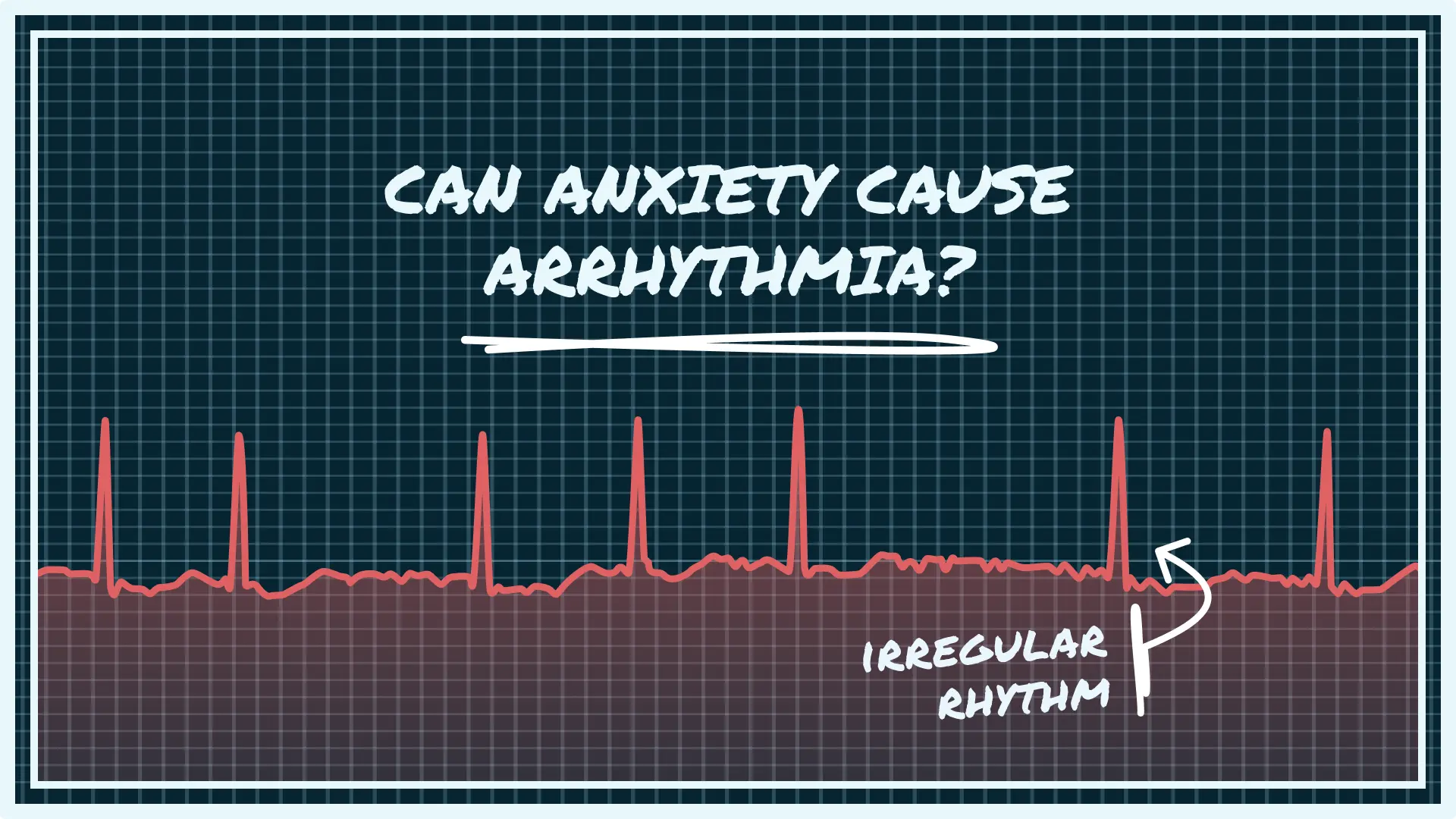
Yes, anxiety can absolutely cause or worsen an arrhythmia. You're not alone in feeling this unsettling connection between a racing mind and a fluttering heart. Understanding why it happens is the first powerful step toward feeling more in control of your body and your well-being.
Your Guide to Anxiety and Heart Rhythms
We get it. Navigating health concerns can be confusing and frustrating, especially when you feel like your worries aren't being taken seriously. This guide is a safe space to gently unpack the connection between your emotions and your heart’s rhythm.
Our goal is to arm you with clear, trusted information. We want to help you learn the difference between anxiety-induced flutters and symptoms that might need a closer look from a doctor, so you can feel confident in your own health journey.
What Is an Arrhythmia Anyway?
Before we dive deeper, let’s get clear on what an arrhythmia actually is. Think of your heart as having a natural, built-in pacemaker. It’s responsible for keeping your heart beating in a steady, predictable rhythm.
An arrhythmia is simply any change from this normal rhythm.
It doesn’t always mean something is seriously wrong. The rhythm might just be:
- Too fast (what doctors call tachycardia)
- Too slow (known as bradycardia)
- Irregular or chaotic (like a skipped beat or a flutter)
Many arrhythmias are harmless, but the sensations they cause can be genuinely frightening. This is where that powerful connection to anxiety comes into play.
An arrhythmia is an irregular heartbeat. It happens when the electrical signals that coordinate the heart's beats don't work properly. While some arrhythmias are harmless, others can be bothersome or even life-threatening.
How Anxiety Triggers Your Heart
When you feel anxious, your body can't tell the difference between a stressful work deadline and a real, physical threat. It flips a switch on your ancient "fight-or-flight" response, flooding your system with stress hormones like adrenaline.
This hormonal surge is designed for survival. It directly impacts your heart, telling it to pump faster and harder to send blood to your muscles so you can react.
Sometimes, this chemical jolt can interfere with the heart's delicate electrical system, causing those flutters, skipped beats, or racing sensations you feel. It's a real, physical response to an emotional trigger.
Understanding the Science of the Heart-Mind Connection
It can be incredibly unsettling when an anxious thought triggers such a powerful physical reaction in your heart. Let's pull back the curtain on this process. This isn't some strange mystery; there's clear science that explains exactly how your mind can directly influence your heart's rhythm.
At the core of this connection is your body's "fight-or-flight" response. Think of it as a super-sensitive internal alarm system, hardwired to protect you from danger. When you feel anxious or stressed, your brain doesn't really know the difference between a real, physical threat and a perceived one, it just sounds the alarm.
Your Body on High Alert
This alarm kicks off the release of potent stress hormones, and adrenaline is the most famous of the bunch. Adrenaline is like an emergency fuel injection for your body. It instantly gets you ready to either confront or escape danger by revving up your heart rate and increasing the force of its contractions.
This sudden hormonal surge talks directly to your heart's electrical system. Imagine your heart's natural pacemaker, which normally keeps a steady, reliable beat, suddenly getting zapped with extra electricity. This jolt can easily disrupt the stable rhythm, causing it to become erratic. This is precisely why so many people ask, "can anxiety cause arrhythmia?" The link is direct and physical.
More Than Just Feelings
The impact of emotional stress on the heart is well-documented and very real. In fact, scientific analysis estimates that approximately 20-40% of sudden cardiac deaths are triggered by acute emotional stressors like intense anxiety or anger. These powerful emotions can create dangerous electrical instability in the heart, showing just how significant this connection truly is.
"Your racing heart isn't 'all in your head.' It's a real, physical response to the stress hormones released by your brain during anxiety. Acknowledging this connection is the first step toward managing it.
Another fantastic metric is your Heart Rate Variability (HRV). It measures the tiny variations in time between each heartbeat and serves as a great indicator of your nervous system's balance. To learn more, you might be interested in our guide on what is heart rate variability.
Identifying Common Arrhythmias Linked to Anxiety
When your heart does something out of the ordinary, the feeling can be incredibly unsettling. But it helps to know that not all heart flutters feel the same, because not all arrhythmias are the same. Putting a name to what you're feeling can be a powerful first step in taming the fear of the unknown.
The goal here isn't self-diagnosis, but recognition. When you can describe the specific sensations you're having, you can have a much more confident and productive conversation with your doctor. It helps them take your concerns seriously and get to the bottom of it faster.
Benign but Bothersome Beats
For many people dealing with anxiety, the most common culprits are often benign (meaning harmless) arrhythmias that can still feel pretty alarming. They're usually brief and feel like a sudden, jarring interruption in your heart's otherwise steady rhythm.
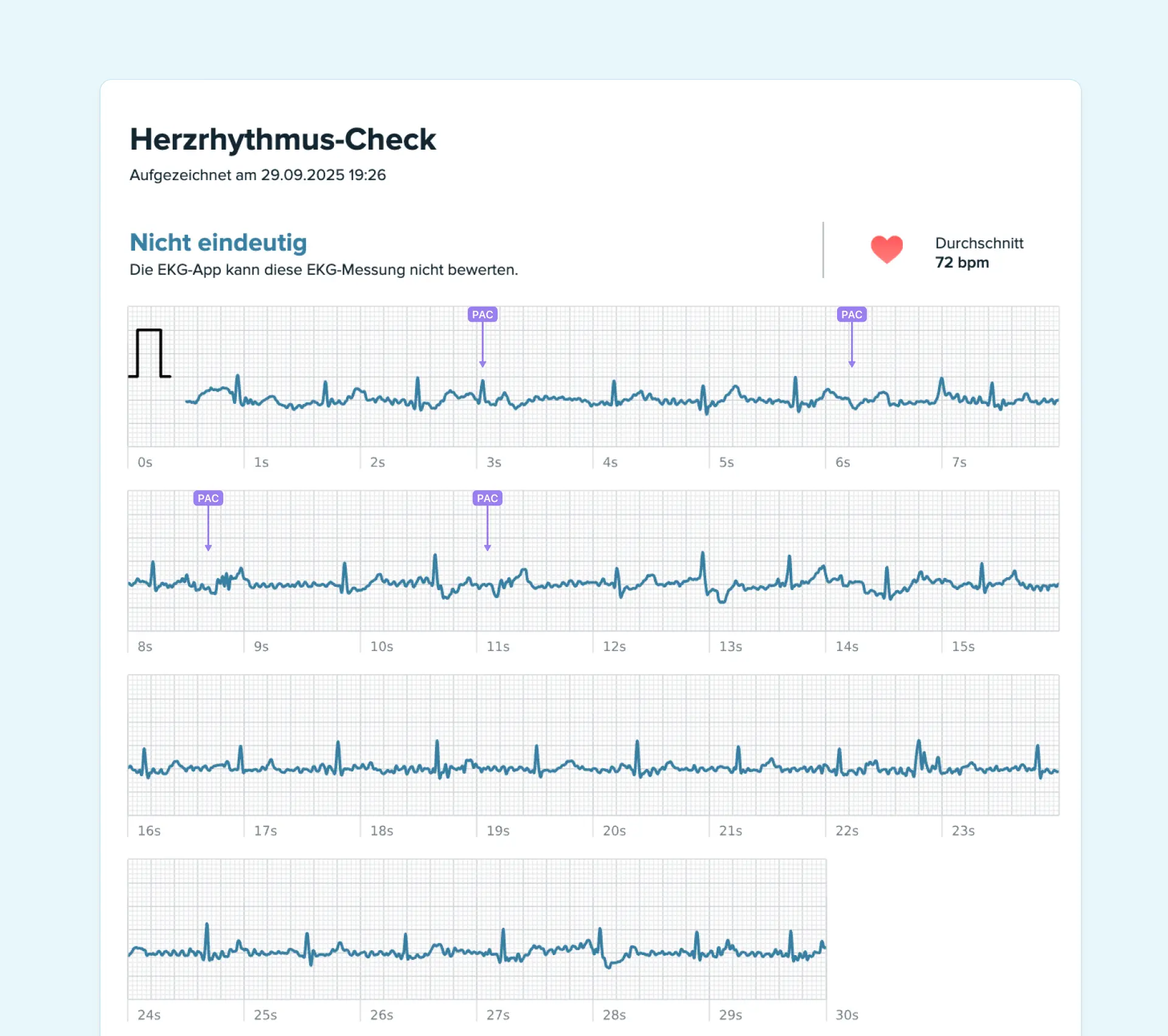
- Premature Atrial Contractions (PACs): These are early beats that kick off in the atria, your heart's upper chambers. People often describe them as a little flutter or a "skipped" beat, which is then followed by a slightly more forceful beat.
- Premature Ventricular Contractions (PVCs): Much like PACs, these are early beats, but they start in the ventricles, the lower chambers. The sensation is often described as a "hiccup" in the chest, a flip-flop feeling, or a single, sudden thump that gets your attention.
It's important to remember that almost everyone has PACs and PVCs now and then. The catch is that anxiety and stress can make them happen more often, or simply make you more aware of them. This can easily kickstart that vicious anxiety-palpitation cycle.
When the Rhythm Is More Sustained
Sometimes, the change in your heart's rhythm isn't just a single odd beat but a longer-lasting episode. These can feel more intense and are important to recognize, as they may require more attention.
Atrial Fibrillation (AFib) is one of the most significant arrhythmias that has a strong link to stress. This is where the heart's upper chambers start beating chaotically, completely out of sync with the lower chambers. The sensation is often described as a quivering or an intensely irregular, rapid heartbeat. Studies have shown that over 40% of people diagnosed with AFib also have anxiety, highlighting a powerful connection. The constant "fight-or-flight" response from chronic anxiety can put a real strain on the heart, potentially contributing to the condition.
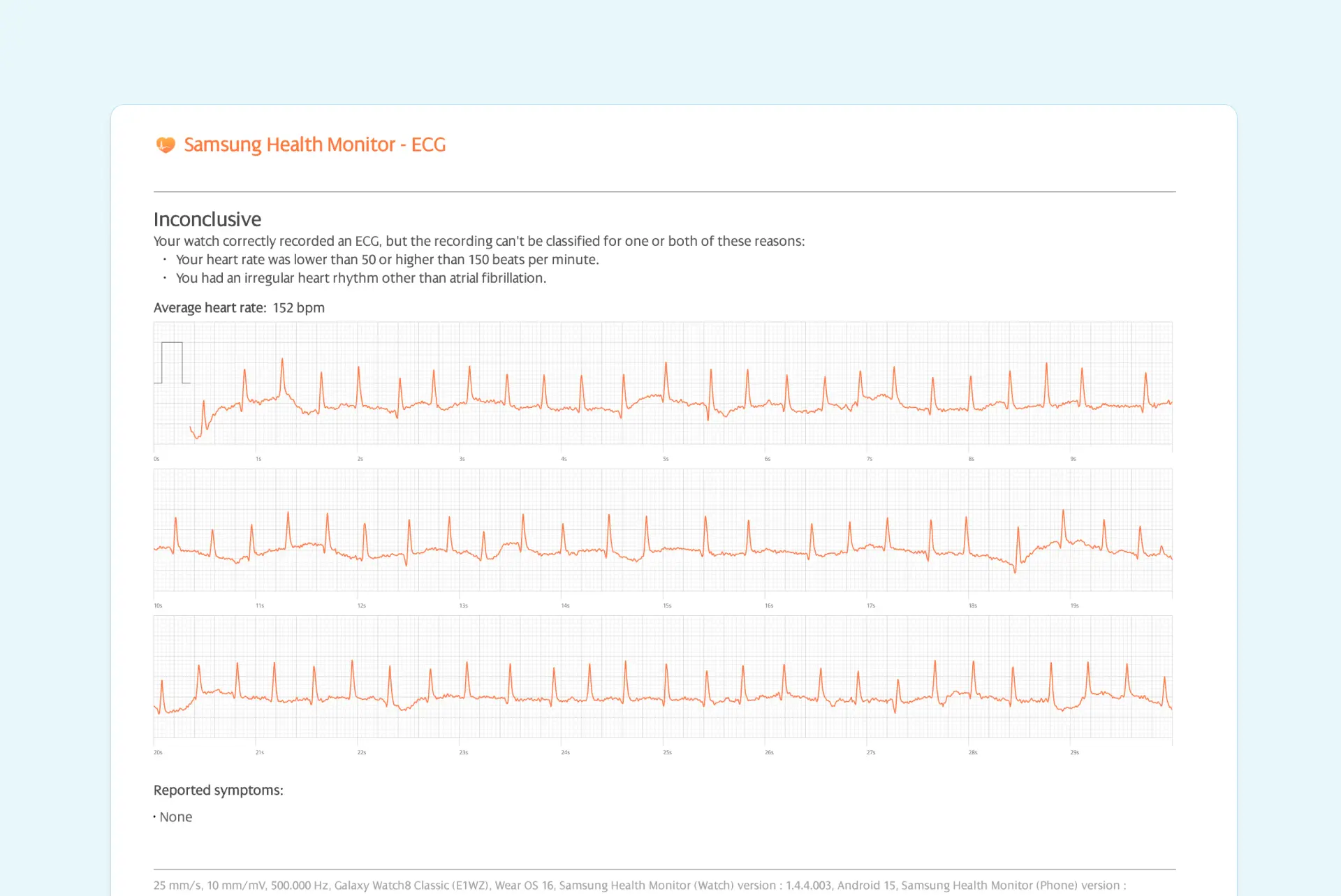
Another one you might encounter is Supraventricular Tachycardia (SVT). This isn't usually an irregular rhythm, but an abnormally fast one. SVT involves episodes of a very rapid but regular heartbeat that can start out of nowhere and stop just as suddenly. It often feels like a switch was flipped, sending your heart racing for minutes or sometimes even hours.
Understanding how stress can be a trigger for conditions like AFib is a crucial piece of the puzzle. You can learn more about managing AFib from stress in our detailed article.
Breaking the Vicious Cycle of Anxiety and Palpitations
It’s an incredibly frustrating experience, a powerful loop that can feel impossible to escape. Your anxiety sparks a heart flutter, and that alarming physical sensation immediately kicks off even more anxiety. We want you to know this is a real, recognized phenomenon, and you are absolutely not alone in it.
The moment you feel that unexpected palpitation, your mind can instantly leap to the worst-case scenario. This fearful thought acts like a siren, flooding your body with another wave of stress hormones. This new surge often provokes more palpitations, which in turn seems to confirm your initial fear that something is terribly wrong.
It quickly becomes an echo chamber where the physical feeling and the mental fear feed off each other. But here's the good news: understanding this feedback loop is the first and most critical step toward breaking it.
The Psychology of the Feedback Loop
This cycle isn't just a vague feeling; it's a well-understood psychological and physical process. It often starts with a heightened awareness of your body's sensations, something very common in people who deal with anxiety. You're already on high alert, so you're far more likely to notice a minor heart flutter that someone else might not even register.
Once you notice it, your anxious brain flags it as a threat. This sets the self-perpetuating cycle in motion:
- Initial Trigger: A moment of stress or anxiety causes a minor palpitation.
- Catastrophic Thinking: Your mind immediately interprets the flutter as a sign of a serious heart problem.
- Physical Reinforcement: This scary thought triggers an even stronger fight-or-flight response, releasing more adrenaline.
- Worsening Symptoms: The adrenaline rush causes more frequent or stronger palpitations, which feels like proof that your initial fear was right.
This cycle can make you feel powerless, but simply recognizing it as it happens is a powerful tool. It allows you to step back and reframe the situation: "Okay, this is the anxiety loop, not a heart attack."
Clinical studies on arrhythmias confirm just how much anxiety can worsen heart rhythm disturbances. The research shows that the toll anxiety takes on a person's quality of life can be just as significant as depression, which is why tackling the mental health side of heart palpitations is so important. You can see the data for yourself in the full research on anxiety and arrhythmia.
Taking the First Steps to Break Free
Learning how to interrupt this cycle is the key to regaining a sense of calm and control. It begins with challenging those automatic negative thoughts that pop up right after a palpitation.
For anyone looking for professional guidance, exploring therapeutic support can be a game-changer. There are many accessible online therapy options that provide proven tools to help you manage these exact thought patterns. By addressing the anxiety directly, you weaken the very trigger that starts the loop in the first place.
How to Prepare for a Productive Doctor's Visit
It's true that anxiety can cause arrhythmias, but it’s still critical to see a doctor to make sure nothing more serious is going on. We get it, this can be an intimidating step, especially if you’ve felt dismissed by doctors in the past. But this is about giving you the tools to advocate for yourself and get the answers you need.
The key is to shift your mindset from being a passive patient to an active, prepared partner in your own healthcare. When you document what's happening, you’re providing concrete data that’s much harder for anyone to ignore. It changes the conversation from one about vague feelings to one grounded in clear facts.
Creating Your Symptom Journal
The single most powerful tool you can bring to an appointment is a symptom journal. Don't worry, it doesn't have to be complicated. Every time you feel a palpitation or an unusual rhythm, just jot down a few key details.
Here’s what your journal should include:
- What it felt like: Was it a flutter? A sudden thump? A skipped beat or a racing feeling?
- When it happened: Make a note of the date and time.
- What you were doing: Were you just resting on the couch, exercising, feeling stressed, or waking up?
- How long it lasted: Did it pass in a second, or did it go on for a minute or more?
- Any other symptoms: Did you feel dizzy, short of breath, or anxious at the same time?
Keeping this detailed record helps your doctor spot patterns they might otherwise miss and shows them you're taking your concerns seriously.
By tracking your symptoms, you are building a case for your own health. This data empowers you to lead the conversation, ensuring your experiences are fully understood and properly investigated.
It’s also a great idea to prepare your questions ahead of time. Instead of trying to remember everything on the spot, you'll walk in with a clear list to guide the discussion. For some help with this, check out our guide on the most important questions to ask your cardiologist. This little bit of prep work can make all the difference in leaving the appointment with the clarity and peace of mind you deserve.
Using Heart Monitoring to Find Peace of Mind
Let's be honest, the fear of the unknown is often the scariest part of dealing with heart palpitations. When your heart suddenly flutters or skips a beat, your mind can instantly jump to the worst-case scenario. This is where modern technology can be a game-changer, offering a powerful way to find reassurance and break that vicious cycle of worry.
Think of a personal ECG device as your secret weapon against anxiety. Instead of just guessing what that strange beat was, you can actually capture it the moment it happens. This simple act transforms you from a passive worrier into an active participant in your own health.
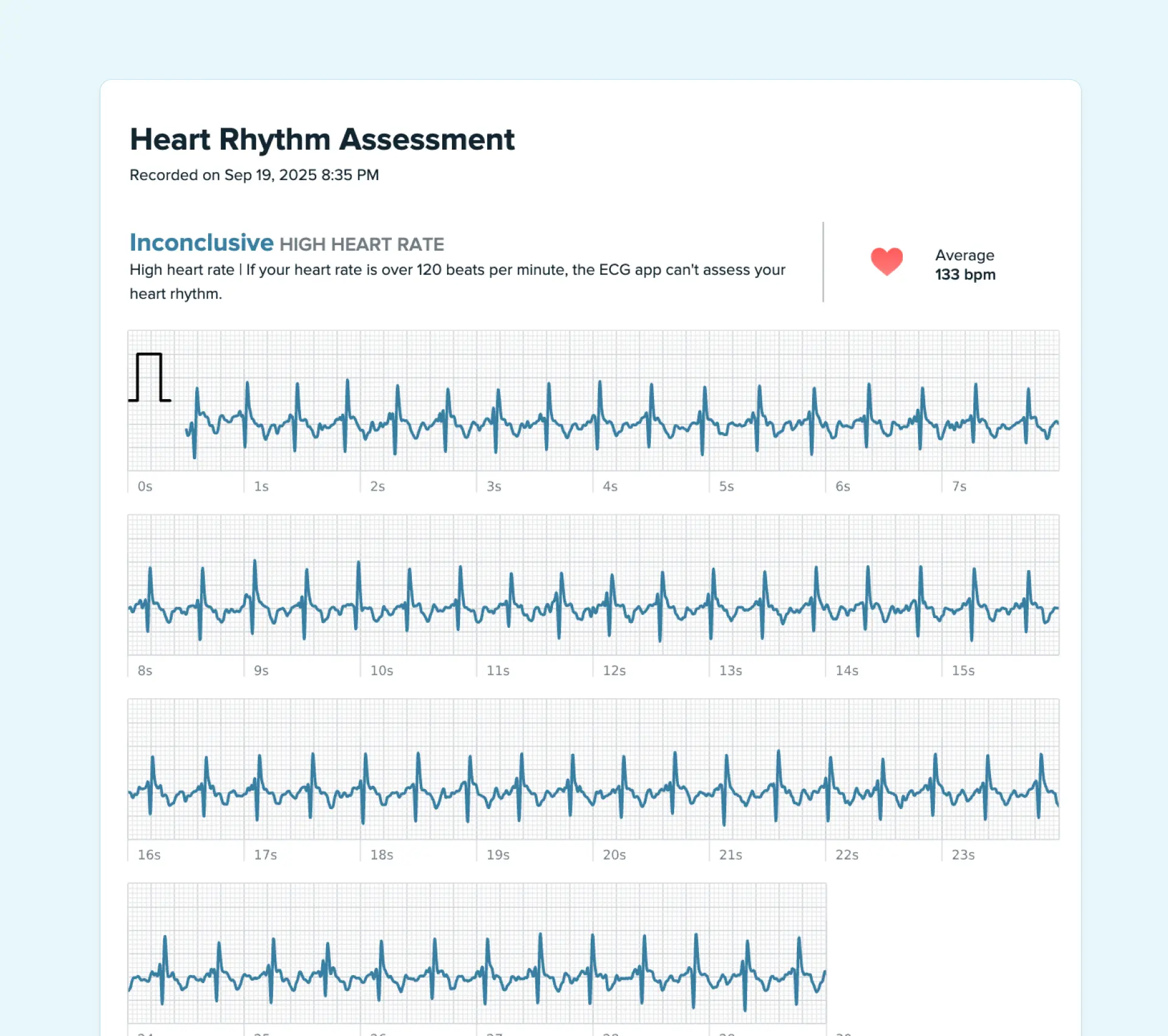
Gathering Your Own Heart Data
The real power here isn't about diagnosing yourself, it's about collecting clear, objective data to silence all those nagging "what ifs." When you feel that flutter, you can record your heart's rhythm on the spot. This recording, your ECG, is a literal snapshot of your heart's electrical activity during the event.
Imagine the relief of turning a moment of panic into a moment of clarity. You’ll have a real piece of data that shows exactly what happened. This information is invaluable because it replaces anxious guesswork with concrete evidence you can share with a professional.
Knowing for certain whether a flutter was a benign PVC or something that needs a follow-up can be life-changing. It replaces anxious speculation with factual understanding, which is a huge step in managing health anxiety.
This process also makes you a much more effective partner in your own healthcare. Armed with your ECG recordings, you can walk into a doctor’s appointment with confidence. You’re not just describing a vague feeling; you’re presenting the very data they need to help you.
Many wearable devices, like the Apple Watch, have made this incredibly simple. If you're new to this, learning how to take an ECG with your Apple Watch is a great first step on your journey toward peace of mind.
Common Questions About Anxiety and Arrhythmia
Digging into the link between your mind and your heart can bring up a lot of questions. Getting clear, practical answers is a huge step toward feeling more in control and less afraid. Let's walk through some of the most common concerns people have.
Can I Stop Anxiety-Related Palpitations Completely?
While aiming to stop them forever might not be realistic, you can absolutely get a handle on them and reduce how often they happen and how intense they feel. The real key is to manage the root cause: the anxiety itself.
Think of it this way: strategies like deep breathing, mindfulness, therapy, and regular exercise all work to calm your nervous system down. This makes your heart less jumpy and reactive to stress. As your overall anxiety level comes down, you'll almost certainly notice the palpitations do, too.
Are Heart Palpitations from Anxiety Dangerous?
For the vast majority of people, heart palpitations caused by anxiety are not dangerous. They're often benign arrhythmias like PVCs or just your heart beating a bit faster than usual for a short time.
That said, it's impossible to know for sure without a proper medical evaluation. If your palpitations are a new thing for you, happen a lot, or show up with other symptoms like dizziness, fainting, or chest pain, it’s vital to see a doctor. The peace of mind that comes from a clear diagnosis is a powerful part of feeling better.
The question, "Can anxiety cause arrhythmia?", is almost always followed by "is it dangerous?" While they're typically harmless, getting a professional opinion to rule out any underlying issues is the safest and most reassuring path. Your peace of mind is non-negotiable.
How Do I Tell an Anxiety Attack from a Heart Problem?
This is a tough one, because the physical symptoms can feel nearly identical, which is incredibly frightening in the moment.
Generally, the symptoms of a panic attack tend to ramp up and peak within about 10 minutes before they start to fade. In contrast, a heart attack often involves more of a constant, crushing pain that might spread to your arm, jaw, or back.
But you should never, ever try to diagnose yourself during an intense event. If you have any doubt at all, the safest and smartest move is always to get immediate medical help.
Feeling anxious about your heart? Qaly experts review your ECGs for irregularities like PACs, PVCs, AFib, and more within minutes. Try it now for peace of mind.









.png)
.png)