Key Takeaways
Hello Heart Hero.
Yes, there is a real connection between vitamin D and heart palpitations. When levels of this vital vitamin dip too low, it can throw off your body's calcium balance and the delicate electrical signals that keep your heart beating steadily. This disruption can absolutely lead to those unnerving flutters and skipped beats. For many people, getting their vitamin D back into a healthy range can help calm their heart rhythm.
Your Guide to Vitamin D and Heart Palpitations

If you’ve ever felt that confusing flutter, sudden skip, or racing beat in your chest, you know how unsettling it can be. Maybe you've been told it's "just stress" or too much coffee, but you have a nagging feeling there's more to it. It’s frustrating when you know something in your body feels off, but you can’t get a clear answer.
This guide is for you. We're going to dig into the often-overlooked link between vitamin D and heart palpitations, going beyond the simple, surface-level explanations. We'll explore what’s actually happening inside your body, how a simple vitamin imbalance could be a piece of the puzzle, and what practical steps you can take to figure it out.
A New Path to Understanding Your Heart
It can feel disheartening when you’re not getting the full picture from the traditional healthcare system. You deserve clear, empowering information that helps you connect the dots for yourself. This guide is built on that idea. We'll explore:
- The Science, Simplified: We'll break down how the "sunshine vitamin" directly influences your heart's rhythm, without the confusing medical jargon.
- The Importance of Balance: You'll learn why both too little and too much vitamin D can cause problems for your heartbeat.
- Actionable Steps: We’ll show you how to investigate this connection for yourself, from getting the right tests to monitoring your symptoms at home.
This isn't about quick fixes or miracle cures. It's about giving you a solid foundation of knowledge.
The goal is to empower you with clear, reliable information so you can have more informed, productive conversations with your doctor. Your concerns are valid, and understanding the potential root causes is the first step toward finding relief.
Our journey together will start with the 'what' and 'why' before moving to the 'how.' We'll look at the physiological role of vitamin D, review the evidence linking it to heart rhythm, and discuss how you can safely take control. By the end, you'll have a much clearer perspective on the link between vitamin D and heart palpitations and feel better prepared to advocate for your own health.
Understanding What Heart Palpitations Really Feel Like
Heart palpitations are a strange and personal experience. For some, it’s a gentle flutter, almost like a butterfly is trapped inside their chest. For others, it’s a forceful pounding that you can feel all the way up in your neck. And then there's that jarring sensation of a sudden pause followed by a hard thump, as if your heart just skipped a beat.
These feelings are your body's way of tapping you on the shoulder. While they're often harmless, they are a definite signal that something deserves a closer look.
Normally, your heart does its job quietly in the background. A palpitation is any change in its speed, rhythm, or force that’s strong enough for you to notice. Understanding what you're feeling is the first step toward figuring out what's causing it.
Common Triggers and Deeper Causes
When you mention palpitations to a doctor, they’ll often run through a list of common culprits, and for good reason. Many everyday things can throw your heart off its rhythm.
- Anxiety and Stress: When you’re wound up, your body floods with hormones like adrenaline, which can easily make your heart race or beat more forcefully.
- Dehydration: Simply not drinking enough water can throw off your body's electrolyte balance, which is crucial for the electrical signals that keep your heart beating steadily.
- Stimulants: That morning coffee, nicotine from smoking, and even certain medications can directly poke at your heart muscle, triggering palpitations.
But what if you've already cut back on coffee, you're drinking plenty of water, and you're managing your stress? This is where your intuition to dig deeper becomes so important. If you’ve addressed the usual suspects and the palpitations continue, it’s often because a quieter, underlying factor, like your vitamin D level, is playing a significant role.
Your body is a complex, interconnected system. A simple deficiency in a key nutrient like vitamin D can disrupt the delicate balance needed for a steady heartbeat, creating the very palpitations that common advice fails to resolve.
When Palpitations Signal an Arrhythmia
It’s helpful to know the difference between the feeling and the diagnosis. "Palpitation" is the word for the sensation you experience, while an arrhythmia is the medical term for an actual irregular heartbeat. So, palpitations are often the main symptom of an arrhythmia. This doesn't mean every flutter is a serious problem; many arrhythmias are perfectly benign.
A very common cause for that "skipped beat" or "thump" feeling is something called an ectopic beat. These are essentially extra heartbeats that arrive a little too early. While they’re usually harmless, they can cause a lot of anxiety. If you have a smartwatch, you can even learn more about how to identify ectopic beats on your Apple Watch ECG to get a better handle on what you might be feeling.
Recognizing that the cause might go beyond just stress or caffeine is a powerful step. It opens the door to exploring other possibilities, like the link between vitamin D and heart palpitations, and empowers you to find a more complete and lasting solution.
The Surprising Role of Vitamin D in Your Heart's Rhythm

It can feel strange to connect a vitamin we get from sunshine to the steady beat of our hearts. But the link between vitamin D and heart palpitations is surprisingly direct. Often called the "sunshine vitamin," it plays a deep role in managing your body's intricate electrical system, and when your levels are off, you can often feel the effects right in your chest.
Think of vitamin D as a skilled traffic controller for calcium, a mineral that's absolutely vital for your heart's function. One of its main jobs is to make sure calcium gets where it needs to go, like into your bones to keep them strong. Just as crucial, it helps keep calcium from building up where it shouldn't, like in your arteries.
But that's not its only job. Vitamin D also helps maintain the delicate balance of electrical signals that tell your heart muscle when to contract and relax. When vitamin D levels dip too low, this whole system can get thrown out of sync. It’s like the traffic controller is off duty, letting the electrical signals get a little scrambled. This kind of disruption can easily lead to the flutters, skips, and pounds we feel as palpitations.
The Calcium Connection
Your heart is a muscle. And like any other muscle, it needs calcium to contract properly. Every single heartbeat is powered by a precise movement of calcium ions flowing in and out of your heart cells. This movement is what creates the electrical impulse that keeps your heart beating in a steady, reliable rhythm.
Vitamin D is the master regulator of this entire process. When your levels are where they should be, your body absorbs and uses calcium efficiently. But when you’re deficient, the system falters.
Without enough vitamin D to guide it, calcium management can become disorganized. This can interfere with the heart’s electrical stability, making it more prone to the kind of irregular beats that cause palpitations.
This isn't just a theory; it's a physiological reality. The muscle cells in your heart actually have vitamin D receptors on them, which is a clear sign of just how important this nutrient is for normal cardiac function.
What the Evidence Shows
It’s one thing to understand the mechanics, but it helps to know this connection is backed by solid scientific observation. Time and again, researchers have found that people with low vitamin D levels often face a higher risk of irregular heartbeats.
For instance, large-scale studies have shown that vitamin D deficiency is tied to a measurable increase in the risk of certain heart rhythm issues. One analysis discovered that having deficient levels (under 20 ng/mL) was associated with about a 12% higher relative risk of developing atrial fibrillation, a very common type of irregular heartbeat. This kind of research validates the gut feeling that many people have, that there’s a deeper cause for their palpitations. You can dive into the findings of this research on vitamin D and heart rhythm on frontiersin.org.
Understanding this science is empowering. It confirms that looking beyond the usual suspects like stress and caffeine is a smart move. There are real, tangible reasons why a nutritional imbalance could be contributing to what you're feeling. Of course, vitamin D is just one piece of the puzzle. You might also be interested in learning about other important vitamins for heart health in our detailed guide. Knowing how these nutrients work together gives you a more complete picture of what your body needs to maintain its natural rhythm.
Let's dive a little deeper into how vitamin D and heart palpitations are connected, but without the confusing medical jargon. When you feel that flutter or skipped beat, it can seem like a total mystery. But understanding that there are real, measurable changes happening inside your heart’s electrical system can be incredibly validating.
It’s not just in your head. Your concerns are rooted in real physiology, and we can actually see these subtle shifts using a tool you might already be familiar with: the electrocardiogram, or ECG.
What an ECG Can Show Us
An ECG is simply a recording of your heart's electrical activity. Think of it like a sound engineer looking at the waveform of a song. Every peak and valley on an ECG tells a specific story about how your heart is beating, from the first electrical spark to the moment the muscle resets for the next beat.
When vitamin D levels are low, this delicate electrical dance can get a little off-key. The changes are often subtle, but they're significant enough to make the heart a bit more "excitable" or prone to firing off-beat. It’s these tiny electrical hiccups that you might feel as palpitations.
One of the key measurements on an ECG is something called the QT interval.
Think of the QT interval as the total time your heart muscle needs to squeeze and then fully recharge before it can beat again. It's a crucial period of action and recovery.
Research has shown that when vitamin D is deficient, this recharge time can get slightly thrown off. This doesn't mean your heart is in immediate danger, but it does mean the electrical environment is less stable, which creates more opportunities for those frustrating palpitations to pop up.
A Closer Look at Your Heart's Recharge Time
Going a step further, scientists can zoom in on even more specific parts of your heart's electrical cycle. Studies have found that people with low vitamin D levels sometimes show measurable changes in how their heart's main pumping chambers, the ventricles, "recharge", a process called repolarization.
Specifically, they've documented changes in ventricular repolarization that point to a connection between deficiency and a higher risk of arrhythmia. One study discovered that people with low vitamin D had longer measurements for something called the Tpeak to end (Tp e) interval, which is a known marker for electrical instability. Basically, the lower the vitamin D, the longer this interval became, suggesting a less stable heart rhythm. You can read more about these electrocardiographic findings on clinmedjournals.org.
This isn’t meant to scare you. On the contrary, it's powerful information that confirms what you're feeling. It shows a direct, plausible link between a simple nutrient deficiency and the very real physical sensations you're experiencing.
The Bigger Electrical Picture
It's helpful to remember that your heart's electrical system doesn't operate in a vacuum. It relies on a perfect balance of minerals called electrolytes, like calcium, magnesium, and potassium, to work correctly. As we've touched on, vitamin D is the master regulator of calcium.
When vitamin D is low, it can throw this whole mineral balance out of whack. This is a lot like how other mineral imbalances can affect your heart's rhythm. You can explore this connection further by reading our guide on how electrolyte imbalance can affect your ECG.
Understanding this empowers you to have much more productive conversations with your doctor. You can move beyond just saying "I'm having palpitations" and start discussing potential underlying factors, armed with the knowledge that there's real science backing you up. You're not just guessing anymore; you're connecting the dots in your own health story.
Why Too Much Vitamin D Can Also Cause Palpitations
It's a common line of thought: if a little of something is good, then more must be better. But when it comes to your heart's precise electrical rhythm, balance is everything. While low vitamin D gets a lot of attention for its link to palpitations, the other side of the coin is just as important to understand: vitamin D toxicity.
Taking very high doses of supplements, especially when you don't know your current levels, can unfortunately have the opposite of the intended effect. This isn't meant to cause alarm, but to give you the complete picture so you can make safe, smart choices for your heart health.
The Problem of Too Much Calcium
When you take extremely high doses of vitamin D for a long time, it can lead to a serious condition called hypercalcemia. That’s the medical way of saying you have dangerously high levels of calcium in your blood.
Think back to how vitamin D acts as the gatekeeper for calcium absorption. In cases of toxicity, that gatekeeper goes into overdrive, ushering far too much calcium into your bloodstream. And this is where the trouble starts for your heart.
Instead of helping your heart muscle contract smoothly, all that extra calcium becomes a disruptive force. It can mess with your heart’s delicate electrical signaling, making the muscle cells irritable and overly excitable.
This electrical instability can, ironically, trigger the exact same heart palpitations you might have been trying to get rid of. Your heart's steady rhythm relies on a precise mineral balance, and flooding the system with excess calcium throws that balance completely off.
What Does "Too Much" Really Mean?
Let's be clear: vitamin D toxicity is rare. It almost always happens from taking massive doses of supplements over a prolonged period, not from getting sun or eating vitamin D-rich foods. We are not talking about standard daily supplements here.
Clinical reports have shown that long-term intake of extremely high doses, like 60,000 IU per day, can lead to toxicity and the hypercalcemia that triggers palpitations. This is far, far beyond what is normally recommended for supplementation. You can learn more about the link between supplement doses and heart symptoms on ejmoams.com.
This really drives home a critical point: more isn't better. The goal is never to flood your system, but to gently guide it back to its natural, healthy "sweet spot."
The Safest Path Forward Is Testing
The connection between vitamin D and heart palpitations is a two-way street. Both too little and too much can disrupt your heart's rhythm, which is exactly why supplementing blindly is a risky guess.
This is where knowing your numbers becomes your most powerful tool. Before you even consider starting a high-dose supplement, getting a simple blood test to check your vitamin D levels is the smartest and most responsible first move.
Here’s why testing is so critical:
- It gives you a baseline. You can't figure out the right dose if you don't know your starting point.
- It prevents over-supplementing. If your levels are already healthy, taking high-dose supplements could push you into the danger zone of toxicity.
- It allows for a targeted plan. Knowing your exact number lets you or your doctor create a safe, effective strategy to gently bring your levels into the optimal range.
Making an informed decision is always the safest and most effective way to restore your body’s natural balance. It takes you from a place of guessing and hoping to one of clarity and confidence.
A Practical Roadmap for Taking Control
Knowing the why behind the link between vitamin D and heart palpitations is the first step. Now, let's talk about what to do with that knowledge. This is your practical roadmap to move from uncertainty to a clear, reassuring plan.
It's incredibly frustrating to feel dismissed when you bring up symptoms with your doctor. This roadmap is all about gathering your own information, so you can be an active partner in your health journey, not just a passenger.
Step 1: Start with a Simple Blood Test
Before you change a single thing, the first and most critical step is to find out your starting point. You can't navigate without a map, and a simple vitamin D blood test is the best map you can get.
This test measures your 25-hydroxyvitamin D levels, giving you a precise number. It's not a guess; it's hard data about your own body. You'll want to specifically ask your doctor for this test. Knowing your number is the only way to safely address a potential deficiency or confirm that your levels are right where they should be.
Step 2: Optimize Your Levels Safely
Once you have your results in hand, you and your doctor can build a safe, effective plan. The idea is to gently guide your body back into balance, not shock it with massive, unmeasured doses of anything.
A combination of three approaches usually works best:
- Sensible Sun Exposure: Your body is designed to produce its own vitamin D from sunlight. Just 10 to 20 minutes of midday sun on your arms and legs a few times a week can make a real difference, though this varies based on your skin tone and where you live.
- Vitamin D-Rich Foods: Try to work foods like fatty fish (salmon is a great one), egg yolks, and fortified milks or cereals into your diet. It's tough to get everything you need from food alone, but every little bit helps support your overall levels.
- Smart Supplementation: If your levels are genuinely low, a supplement is often the most direct route. A common and effective choice is vitamin D3. The key is working with your provider to figure out the right dose based on your specific test results.
Remember, the goal here is balance. As we've covered, too much vitamin D is just as problematic as too little, potentially triggering palpitations by raising your calcium levels. This is exactly why testing first is non-negotiable, it keeps you safe.
This infographic breaks down how taking too much vitamin D can backfire.
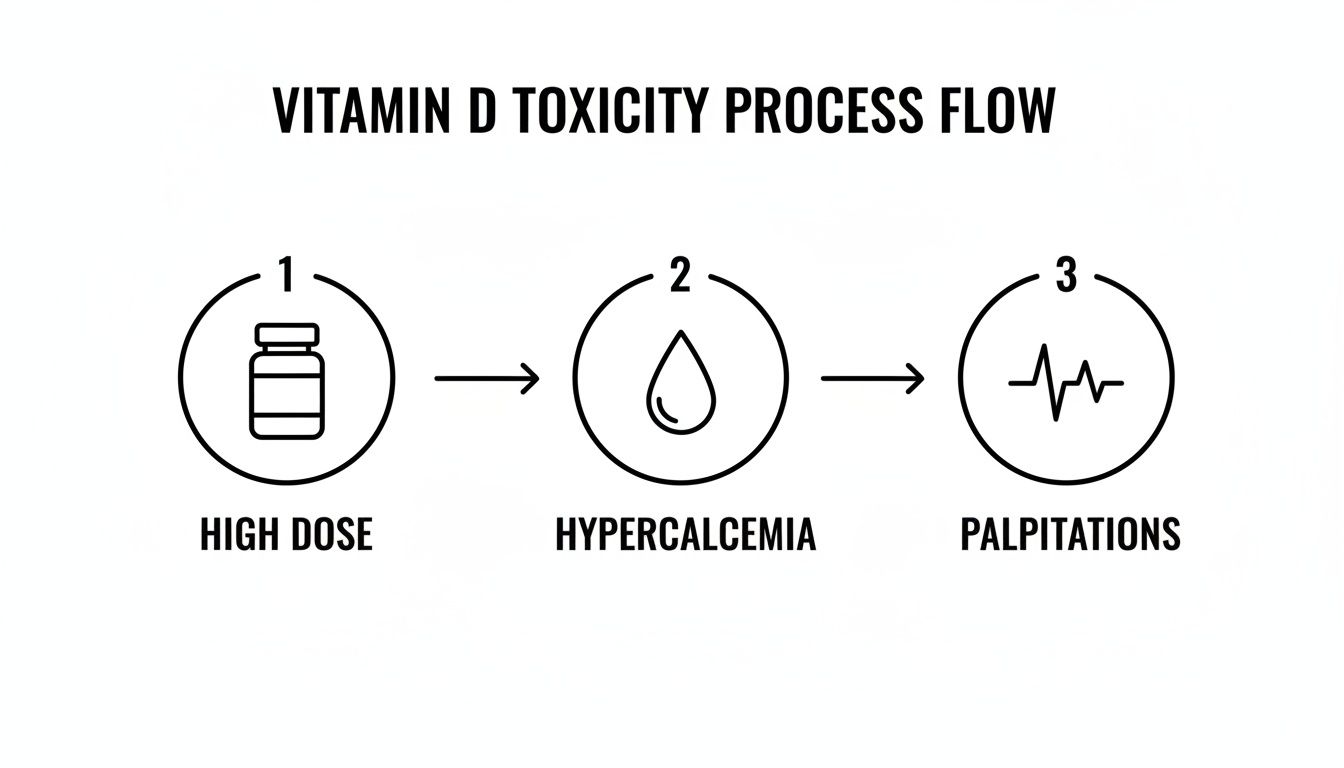
It’s a clear visual reminder that blindly taking high doses can lead to the very symptoms you’re trying to solve.
Step 3: Monitor Your Palpitations at Home
This is where you can really take the driver's seat. Instead of just waiting and wondering if things are improving, you can actively track your heart's rhythm. The ECG function on modern smartwatches (like Apple Watch, Fitbit, or Samsung) lets you capture what you’re feeling, right in the moment it happens.
This is a complete game-changer. Gone are the days of trying to describe a fleeting sensation to your doctor weeks after the fact. You can record an ECG during a palpitation and have actual data to show them. This shifts the conversation from, "I think I felt something strange," to, "Here is the ECG of exactly what I felt."
For even deeper insight, services like Qaly have certified technicians who can analyze those smartwatch ECGs for you. They'll review your recording and provide a detailed interpretation in minutes, helping you make sense of your heart rhythm. It gives you valuable information to track your progress and share with your doctor. And if you're looking for other ways to manage your symptoms, check out our guide on how to stop heart palpitations with top relief tips.
When to Seek Immediate Medical Help
While this guide is about empowering you to investigate the root causes of your symptoms, it's vital to recognize the red flags. If your palpitations come with any of the following, please seek urgent medical care right away:
- Severe chest pain or pressure
- Fainting or feeling like you're about to pass out
- Severe shortness of breath
- Intense dizziness or confusion
These could be signs of a more serious issue that needs immediate attention. Trust your gut. If something feels very wrong, it's always better to be safe and get checked out.
Answering Your Top Questions
We've covered a lot of ground, and it's natural if you still have a few questions. When it comes to your heart health, being thorough is always the right move. Let's tackle some of the most common questions about vitamin D and palpitations with quick, clear answers.
How Soon Can Palpitations Improve After Starting Vitamin D?
There's no one-size-fits-all timeline here. It really hinges on how deficient you were to start and how your individual body responds to supplementation.
Some people report feeling a subtle shift for the better within just a few weeks of consistent use. For others, it can take a few months to fully rebuild their vitamin D stores and notice a significant, lasting change in their heart rhythm. The key is consistent, guided supplementation, not a quick fix.
What Is a Good Vitamin D Level to Aim For?
While lab reports have their own "normal" ranges, a blood level below 20 ng/mL is widely considered a clear deficiency. But many practitioners believe there's a big difference between being "not deficient" and being "optimal."
Many experts suggest an optimal range of 40-60 ng/mL for overall health and to best support a steady, calm heart rhythm.
It's crucial to go over your specific lab results with your doctor. Together, you can set a target range and create a personalized plan that’s right for you.
Do Other Nutrients Help Vitamin D Work Better?
Absolutely. Vitamin D is a team player. Think of magnesium as its most valuable partner, it helps your body actually activate and use vitamin D. Plus, magnesium plays its own direct role in keeping your heartbeat stable.
Another key player is vitamin K2. Its job is to direct the calcium that vitamin D helps you absorb into your bones and teeth, which helps keep it out of your arteries where it could cause problems. A smart approach ensures all these nutrients are working in harmony.
If you're keeping an eye on your heart rhythm at home, you deserve clear, expert analysis of what you're seeing. Qaly provides just that, with certified technicians who interpret ECGs from your smartwatch in minutes.










.png)
.png)