Key Takeaways
Hello, Heart Hero. We hear you. You’re feeling overwhelmed, your heart is doing things that feel scary, and the medical answers you’ve received might feel complicated or even dismissive. It can be a lonely road, especially when you feel like the system isn't listening. But you're not going through this alone, and what you're feeling is very real.
Yes, the connection between AFib and stress is absolutely real - it’s not just "in your head." When your body is under constant pressure, it can throw your heart's natural rhythm out of whack, sometimes triggering the chaotic beat of atrial fibrillation. Getting a handle on this link is the first real step toward regaining control over your heart health and finding solutions that work for you.
The Stress-AFib Connection: Your Body's Hidden Story
Let's break down what's happening inside your body in simple terms. Think of your heart's natural rhythm as a perfectly timed orchestra, with each beat playing its part in harmony. Now, picture stress as a disruptive guest who suddenly crashes the stage.
This guest (stress) unleashes a flood of hormones like adrenaline, signaling your body to kick into "fight-or-flight" mode. This is great in short bursts, like when you need to slam on the brakes in traffic.
But when stress becomes a constant companion from work, family life, or health worries, that internal alarm system never shuts off. This sustained state of high alert is where the trouble starts for your heart's orchestra.
How Chronic Stress Disrupts Your Heart's Rhythm
That constant flood of stress hormones can directly irritate your heart's delicate electrical system. It makes the heart cells (the "musicians" in our orchestra) more excitable and much more likely to start firing out of sync.
Instead of a steady, coordinated beat, you get a chaotic, quivering rhythm. That, right there, is the essence of atrial fibrillation (AFib). The top chambers of your heart (the atria) are no longer pumping blood effectively, which leads to that fluttering or racing sensation you might be feeling.
Let's look at how the body's stress response directly affects your heart's rhythm.
How Your Body's Stress Response Impacts Your Heart
As you can see, what starts as a protective mechanism can become a major disruptor when it doesn't switch off.
You Are Not Imagining It
We know it can feel like you're not being taken seriously, but the medical community is finally catching up and recognizing the powerful link between psychological stress and AFib. In fact, stress is now seen as a major player in both triggering and worsening atrial fibrillation.
Consider this: about one in three people globally reports feeling psychological stress, which can be a direct trigger for an AFib episode. This isn't just about big, traumatic events, either. The slow, steady burn of daily anxiety can be just as impactful.
It can even show up in subtle ways your body responds to stress. If you're curious to learn more, check out our guide on what is heart rate variability, a key indicator of how well your body is coping. Recognizing these patterns is a powerful first step toward feeling in control again.
What AFib From Stress Actually Feels Like
When you're dealing with atrial fibrillation, especially when you think stress is the culprit, the physical sensations can be both confusing and downright scary. Your doctor might give you a clinical checklist of symptoms, but that hardly captures the raw, personal experience of what's happening inside your chest. Let's translate those textbook definitions into what you're actually feeling.
Many people describe AFib from stress as a sudden, chaotic fluttering. It's often compared to the feeling of a trapped bird or a quivering fish in your chest. This isn't just your heart beating fast; it's a completely irregular, unpredictable rhythm that just feels wrong. One moment, your heart is beating along normally, and the next, it’s launched into an erratic drum solo without any warning at all.
This experience can be deeply unsettling, making you feel anxious and suddenly hyper-aware of every single beat. You might feel a hard, out-of-place "thump" that seems to knock the wind out of you, quickly followed by a frantic, racing pace. For others, it’s a more subtle sensation - a persistent quiver or a general feeling of unease that you can’t seem to shake.
Is It Stress or Is It AFib?
It’s tempting to brush these feelings off as "just stress" or normal heart palpitations. In fact, many well-meaning people, sometimes even doctors, might suggest you do just that. But there’s a critical difference between the two, and your intuition is likely spot on.
- Stress Palpitations: These usually feel like your heart is simply pounding hard or beating very fast. You might feel a skipped beat here and there, but the overall rhythm tends to stay pretty steady - just sped up. Once the stressful moment passes, they typically fade away.
- Atrial Fibrillation: AFib is all about irregularity. The rhythm isn't just fast; it’s completely chaotic and unpredictable. The beat can jump from fast to slow and back again in a matter of seconds. Crucially, the feeling often lingers long after the initial stressor is gone.
This ECG from Kardia deviceprovides a clear view of what this looks like. It illustrates how a wearable device can record the electrical tracing of your heart rhythm, simplifying the identification of different types of palpitations.
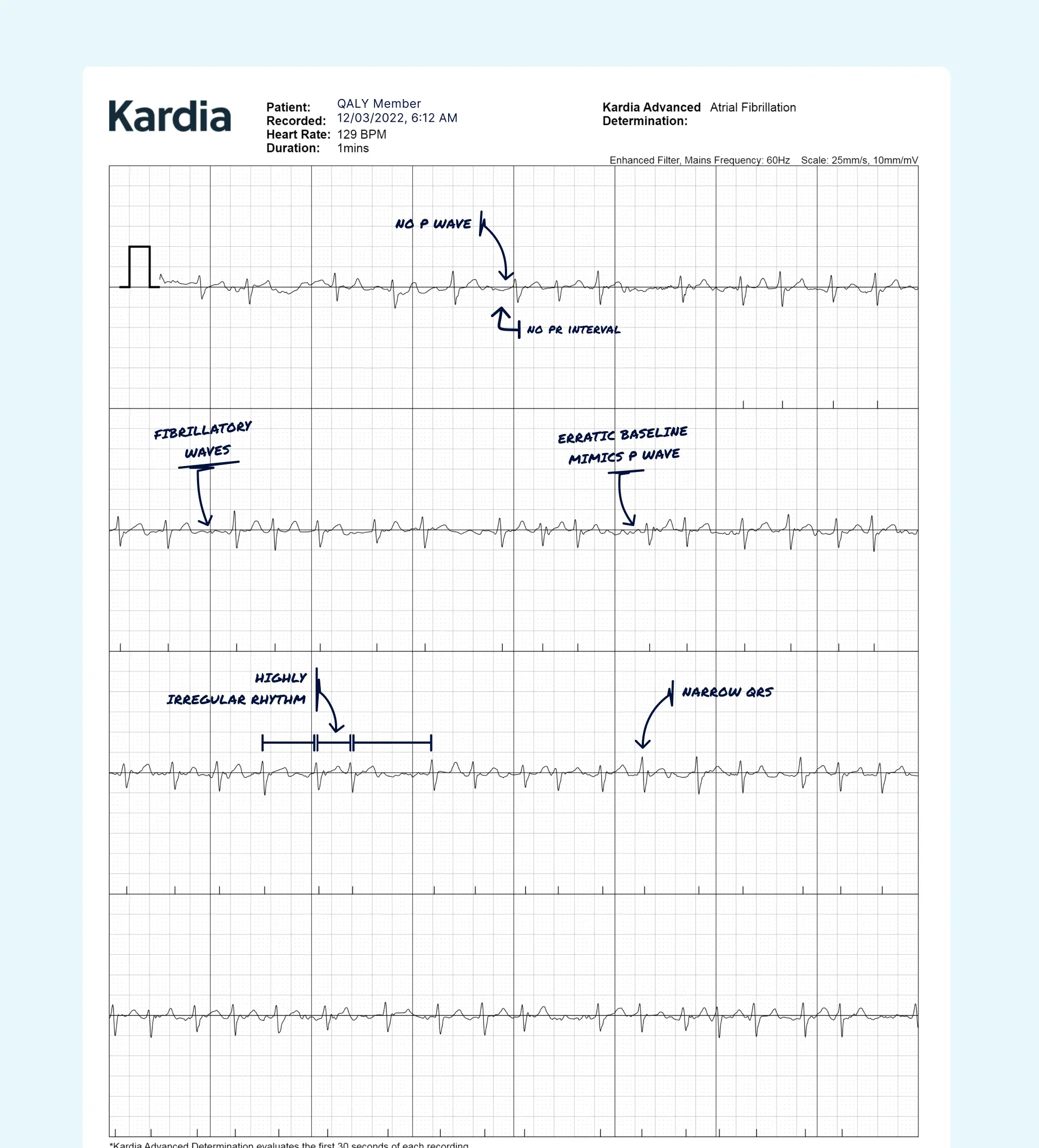
Being able to see your heart's activity in black and white provides real data. It takes you beyond just describing a feeling and gives you concrete information to better understand your body’s signals and advocate for yourself.
The Frustrating Feedback Loop
One of the most challenging parts of AFib from stress is the vicious cycle it can trigger. A stressful event sets off an episode, which, understandably, makes you anxious about your heart. That new anxiety then becomes another stressor, which can make the episode last longer or even kick off a new one.
This feedback loop (where the fear of the symptom becomes a trigger for the symptom) is incredibly common. Recognizing this pattern isn't a sign of weakness; it's the first and most crucial step toward breaking the cycle and regaining a sense of control over your body.
On top of the chest sensations, these episodes can bring on a whole wave of other symptoms. You might suddenly feel dizzy, lightheaded, or short of breath, like you've just run up a flight of stairs while sitting perfectly still. An overwhelming, bone-deep fatigue often follows, leaving you feeling completely wiped out long after your heart rhythm has returned to normal.
Identifying Your Personal AFib Stress Triggers

Stress isn't a one-size-fits-all problem; it’s a deeply personal experience. Just as each of our lives is unique, so are the things that set off our body's stress response. Understanding what triggers afib from stress for you is a bit like becoming a detective for your own heart. It's the key to shifting from feeling powerless to being proactive.
Your triggers might not always be the obvious ones. For some, it’s the sudden jolt of bad news or a heated argument. For others, it's the slow, steady burn of work pressure, financial worries, or the emotional weight of caring for a loved one. Both types of stress can be equally powerful disruptors for your heart's rhythm.
This is where you can start connecting the dots between your daily life and your heart's behavior. By paying close attention, you can uncover patterns that might have been hiding in plain sight. This knowledge empowers you to anticipate and manage potential episodes before they even start.
The Different Faces of Stress
Not all stress feels the same, and different kinds can affect your heart in different ways. It’s helpful to think about them in a few key categories. You might find one is a bigger factor for you than the others.
- Sudden Emotional Stress: This is that jolt from an unexpected event - a sudden loss, a confrontation, or even a moment of intense fear. It causes a rapid spike in adrenaline that can immediately knock your heart out of rhythm.
- Chronic Mental Stress: Think of this as the persistent, low-grade pressure that grinds you down over time. It could stem from a demanding job, relationship issues, or long-term financial anxiety. This constant state of alert keeps stress hormones elevated, creating a vulnerable environment for your heart.
- Physical Stress: Don’t forget that physical strain is also a major stressor. This could be anything from a severe illness or recovering from surgery to simple over-exhaustion from a lack of sleep. It drains your body's resources, making it harder for your heart's electrical system to stay stable.
Identifying which types of stress most influence you is the first step in creating a defense plan. It allows you to determine where to concentrate your efforts for the greatest effect on your well-being.
Becoming a Detective for Your Heart
The absolute best way to identify your unique triggers is to start tracking them. You don't need a complicated system; a simple notebook or a notes app on your phone is all it takes to become your own health investigator. This practice helps turn vague feelings into concrete data.
When you feel an episode start, or just feel generally stressed, try to jot down a few notes. Ask yourself these questions:
- What was I doing right before this started? (e.g., arguing with my partner, rushing to meet a deadline)
- What was I thinking or feeling? (e.g., worried about bills, angry about a comment, sad about a memory)
- How did I sleep last night? (e.g., restless, woke up multiple times, slept like a log)
- What have I eaten or drank recently? (e.g., a big meal, extra coffee, alcohol)
Over time, your journal will start to reveal your personal stress-AFib patterns. You might discover your heart is most vulnerable after a poor night's sleep is combined with a high-pressure work meeting. This insight is incredibly powerful.
Research confirms just how specific these triggers can be. One large-scale study on women found powerful connections between AFib and financial stress, traumatic life events, and even neighborhood stress. Traumatic events had the strongest link, making women who experienced them about 37% more likely to have AFib.
This isn't about blaming yourself or trying to avoid life's challenges. It's about gathering knowledge so you can build resilience and give your heart the support it needs when it's most vulnerable.
How Doctors Diagnose AFib and How You Can Help
Trying to explain that fleeting, chaotic flutter in your chest to a doctor can be maddening. You walk into the clinic, and suddenly your heart decides to behave perfectly. It’s a common story, and it can leave you feeling dismissed and frustrated. But you're not powerless in this situation.
Understanding the diagnostic process, and, more importantly, how you can become an active partner in it is the key to getting the clarity you need. Let’s pull back the curtain on how doctors typically look for AFib and show you why your own observations are so critical.
The Standard Medical Playbook
When you mention symptoms like a racing heart or palpitations, your doctor usually turns to a few standard tools to see what's going on. These tests give them a snapshot of your heart's electrical system and physical structure.
- Electrocardiogram (ECG or EKG): This is almost always the first step. Electrodes are placed on your chest for a few minutes to record your heart’s electrical signals. The big catch? It only sees what your heart is doing right then and there. If you’re not in AFib during those few minutes, the ECG will come back normal, which can be a real letdown.
- Holter or Event Monitor: If the in-office EKG is clean, your doctor might send you home with a wearable monitor. A Holter monitor records everything nonstop for 24-48 hours. An event monitor is worn for longer, but you have to push a button when you feel symptoms to start a recording. They’re better at catching those on-and-off episodes, but can still miss AFib if it’s infrequent.
- Echocardiogram: Think of this as an ultrasound for your heart. It doesn't actually detect AFib, but it checks for underlying structural problems like damaged valves or issues from high blood pressure that could be causing it.
These tests are essential, but they often miss the full picture, especially if you’re dealing with afib from stress that pops up unpredictably. This is where you can step in.
Your Secret Weapon: At-Home Monitoring
This is where you can truly take charge. The single biggest hurdle in diagnosing AFib is capturing an episode while it's actually happening. Since stress-induced AFib can come and go in a flash, the odds of it showing up during a scheduled medical test are pretty slim.
This is why your at-home monitoring is the missing piece of the puzzle.
Modern smartwatches and personal ECG devices have completely changed the game. They put the power to record an ECG right on your wrist, exactly when you feel that strange flutter. Instead of just telling your doctor what you felt, you can show them the data.
Bringing concrete ECG recordings from your own device to an appointment is one of the most powerful things you can do. It transforms your personal experience into objective evidence that a doctor can't ignore, helping to connect the dots between your stress triggers and your heart’s response.
Taking this proactive role works. Apps like Qaly, for instance, let you send your at-home ECGs to certified cardiac technicians for review within minutes. This gives you immediate insight and a professional report you can take directly to your doctor. It helps build a stronger, more collaborative relationship with your care team.
Your Action Plan to Manage Stress and Protect Your Heart
Knowing your triggers is one thing, but having a real playbook to manage them is another entirely. This is your action plan for taking back control. Let's forget the generic advice to "just relax." Instead, we'll walk through practical, science-backed strategies designed to calm your nervous system and support your heart.
Think of these not as chores to add to your already-full plate, but as powerful tools you can reach for anytime you need to restore balance. They work by directly stepping into the stress response cycle, helping your body shift from that frantic "fight-or-flight" mode back to a state of rest and recovery.
Here’s how you can start building a more resilient heart, one small step at a time.
Master the Power of Your Breath
When stress hits, your breathing instinctively becomes shallow and rapid, which is your body's way of signaling to your brain that you're in danger. The good news? You can consciously break this cycle. Intentional breathing is one of the fastest ways to tell your nervous system that everything is okay.
Diaphragmatic breathing, often called "belly breathing," is a simple yet profound technique.
- Find a comfortable position, either sitting or lying down.
- Place one hand on your chest and the other on your belly.
- Breathe in slowly through your nose for a count of four. Your goal is to feel your belly expand like a balloon while your chest remains relatively still.
- Hold your breath gently for a count of two.
- Exhale slowly through your mouth for a count of six, feeling your belly fall.
Try this for just 3-5 minutes a day or anytime you feel that familiar tension rising. This simple act sends a powerful message to your brain that it's safe to stand down, which in turn helps regulate your heart rhythm.
Cultivate Mindful Awareness
Mindfulness is simply the practice of paying attention to the present moment without judging it. When you're caught in a stress spiral about afib from stress, your thoughts are often racing about what already happened or worrying about what might happen next. Mindfulness gently pulls you back to the here and now.
And no, this doesn't mean you need to sit in silent meditation for an hour. You can practice mindfulness anywhere.
- Mindful Morning Coffee: Instead of scrolling on your phone, focus completely on your drink. Notice the warmth of the mug, the rich aroma, and the actual taste of each sip.
- The 5-4-3-2-1 Grounding Technique: When anxiety spikes, just pause. Name 5 things you can see, 4 things you can feel, 3 things you can hear, 2 things you can smell, and 1 thing you can taste. This simple trick yanks your focus away from racing thoughts and plants you firmly in your immediate environment.
Embrace Gentle Movement
Physical activity is a fantastic stress reliever, but we also know that intense exercise can sometimes be a trigger for AFib. The key is to find gentle, consistent movement that calms your nervous system rather than revving it up.
Consider adding one of these to your weekly routine:
- Yoga: A perfect combination of physical postures, breathing exercises, and meditation to reduce stress and improve heart health.
- Tai Chi: Often described as "meditation in motion," this ancient practice uses slow, flowing movements to promote calm.
- Walking in Nature: It's been shown that spending time outdoors can lower cortisol levels and blood pressure. A simple 20-minute walk can make a huge difference.
These activities help your body process stress hormones and release endorphins—your body's natural mood elevators - without putting excessive strain on your heart.
The link between our mental state and heart rhythm is becoming increasingly clear. Researchers now know that mental and emotional stress (from work strain to negative emotions like anger) are significant risk factors for AFib. Brain areas that regulate stress, like the amygdala, can directly influence heart rhythm, highlighting why managing your mental well-being is a core part of comprehensive heart care.
Prioritize Your Lifestyle Foundations
Finally, managing stress isn't just about what you do in a moment of crisis. It's about building a foundation of well-being that makes you less vulnerable to triggers in the first place. Two of the most important pillars of that foundation are sleep and nutrition.
Getting 7-9 hours of quality sleep is non-negotiable for a healthy heart. Poor sleep throws your hormones out of whack and makes your body much more susceptible to stress. Simple changes, like setting a consistent bedtime and avoiding screens an hour before you turn in, can drastically improve your sleep quality.
Similarly, what you eat truly matters. Small nutritional shifts can support your nervous system. For a deeper dive into how your daily habits can protect your heart, check out our guide on atrial fibrillation lifestyle changes. These aren't about adding more rules to your life, but about nourishing your body so it's better equipped to handle whatever stress comes your way.
When to Seek Immediate Medical Help
Hello, Heart Hero. While getting a handle on AFib from stress is a massive step in feeling like you're in the driver's seat, it’s just as critical to know when your body is sending up a flare.
Think of it this way: knowing these red flags is part of your safety toolkit. Reaching out for urgent help isn't a failure or a step back. It’s a smart, powerful move that shows you're your own best health advocate.
Don't Brush These Symptoms Off
If you feel any of the following, it's time to call 911 or head to the nearest emergency room. No hesitation. These are signs that AFib might be causing a serious, immediate problem for your heart or brain.
- Severe Chest Pain: This isn't just a minor ache. We're talking about a crushing, squeezing pressure, or pain that radiates to your arms, back, neck, or jaw.
- Serious Trouble Breathing: Feeling so breathless you can't get a full sentence out, even when you're just sitting still.
- Fainting or Extreme Dizziness: That terrifying feeling like the room is spinning and you're about to pass out, or actually losing consciousness.
These are critical signals that your body needs medical backup, and fast.
Always trust your gut. If a symptom feels intensely wrong or completely different from your usual AFib sensations, it's always better to get it checked out. You know your body better than anyone.
Recognizing the Signs of a Stroke
One of the biggest risks with AFib is the potential for a stroke. The F.A.S.T. acronym is a simple, powerful tool to help you spot the signs in yourself or someone else.
- F - Face Drooping: Ask the person to smile. Does one side of their face droop or look uneven?
- A - Arm Weakness: Ask them to raise both arms. Does one arm drift downward or feel numb?
- S - Speech Difficulty: Is their speech slurred, strange, or are they unable to speak at all?
- T - Time to call 911: If you notice any of these signs, even if they seem to go away, call for help immediately. Every second counts.
Frequently Asked Questions About AFib and Stress
Living with AFib can sometimes feel like you're putting together a puzzle, one piece at a time. Even after learning so much, you might still have a few nagging questions. Let's tackle them head-on, so you can feel more confident and in control of your heart health.
Can Stress Alone Cause AFib in a Healthy Heart?
This is the big one, and the answer isn't a simple yes or no. For most people with a structurally sound heart, a single bad day at work isn't going to suddenly trigger AFib. But chronic, unrelenting stress? That's a different story. It can absolutely create the perfect storm for AFib to develop over time.
Think of your heart’s electrical system as a perfectly paved road. Chronic stress is like a constant, heavy rain that slowly erodes that road, creating potholes and weak spots. Then, one day, a single downpour (a big stressful event) is all it takes for the road to finally give way, leading to an episode of AFib from stress. So, while one event might be the final trigger, the underlying vulnerability was built up over a long period.
Will Reducing My Stress Make My AFib Disappear?
For many, getting a handle on stress can dramatically reduce the frequency and severity of AFib episodes. It's truly one of the most powerful lifestyle changes you can make, and its impact is often much bigger than people expect.
That said, it isn't always a magic cure that makes AFib vanish forever, especially if other things like high blood pressure or sleep apnea are part of the picture. The best way to look at it is this: managing stress is a crucial pillar in your overall heart health strategy. It helps quiet the electrical "noise" in your heart, making it a much less welcoming place for an AFib episode to start.
When you take control of your stress response, you are actively creating a less hospitable environment for AFib. It's about shifting the odds significantly in your favor, which is a massive victory for your long-term well-being.
What Is the First Thing I Should Do When an Episode Starts?
When you feel that familiar flutter and you know a stress-related episode is kicking in, your first instinct might be to panic. Your number one goal is to interrupt that panic cycle before it starts.
Here’s a simple, immediate action plan:
- Stop and Sit Down: Find a safe, quiet place to sit. This simple act helps prevent dizziness from causing a fall and sends a signal to your body that it’s time to switch gears from "fight or flight" to "rest and digest."
- Focus on Your Breath: Immediately start slow, deep belly breathing. Try inhaling for a count of four, holding for a moment, and then exhaling slowly for a count of six. This is the fastest way to send a "calm down" message directly to your nervous system.
- Record Your ECG: If you have a smartwatch or another wearable device, take an ECG recording right away. Capturing the event gives you and your doctor valuable data for later. It also powerfully shifts your focus from worry to proactive action.
Remember, you aren't helpless when an episode begins. These simple steps put you back in the driver's seat, helping you manage the moment instead of letting the moment manage you.
Get your at-home ECGs analyzed by certified experts in minutes, giving you the clarity and peace of mind you deserve.










.png)
.png)