Key Takeaways
Hello Heart Hero.
A heart pacemaker operation is a procedure where a small electronic device is placed under the skin in your chest to help manage a slow or irregular heartbeat. It works by sending tiny electrical signals to the heart, making sure it beats at a steady, healthy rhythm. It's a common and safe procedure that can restore normal heart function and make a huge difference in your quality of life.
Your Guide to the Heart Pacemaker Journey
Hearing you might need a pacemaker can feel like a lot to take in. It is completely normal to feel a mix of emotions and have a million questions running through your mind. We get it, navigating the world of healthcare can be confusing, especially when you feel like just another number. Our goal here is to give you a clear, supportive guide to put you back in the driver's seat.
Think of this as a conversation with a trusted friend, here to walk you through every step with empathy and clear explanations. We want to replace any uncertainty you're feeling with confidence. This guide will break down why your doctor might recommend a pacemaker and what this small but powerful device actually does for your heart. We will cover everything from getting ready for the procedure to what recovery looks like, giving you the knowledge you need to feel prepared.
What We'll Explore Together
We will walk through all the essential information, broken down into simple, manageable pieces. You'll learn about:
- The 'Why' Behind a Pacemaker: Understanding the common heart rhythm issues that a pacemaker can correct.
- Preparing for Your Procedure: Practical steps to help you feel ready and calm beforehand.
- The Operation Itself: A clear, step-by-step overview of what happens during the procedure.
- Life After the Operation: Tips for a smooth recovery and how to thrive with your new device.
This technology has made a massive difference for so many people. In fact, more than 3 million individuals worldwide currently live with a cardiac pacemaker, which has greatly improved their lives by managing irregular heartbeats. These devices are so reliable that major milestones, like the 500,000th pacemaker operation in the UK, show just how vital this technology has become.
We believe that knowledge is empowering. Getting more involved in your own health, like monitoring your heart rhythms, is one way to feel more in control. You can learn more about how to check heart health at home. Our aim is to give you all the information you need, so you can focus on what matters most: your well-being on the path ahead.
Understanding Why You Might Need a Pacemaker
Let's start with a simple analogy. Think of your heart's natural electrical system as the conductor of an orchestra, ensuring every part plays in perfect time to create a steady, rhythmic beat. But what happens if the conductor starts slowing down, losing the tempo, or even misses a cue entirely?
That's when you might feel things like dizziness, constant fatigue, or shortness of breath. A pacemaker is like a reliable backup conductor. It's a small, smart device that quietly observes your heart's rhythm and steps in only when needed to keep the beat steady and strong.
The Main Reasons Your Heart Needs a Backup
Your doctor might bring up a heart pacemaker operation for a few key reasons, all of which trace back to a problem with your heart's internal electrical signals.
The most common issue is bradycardia, which is simply the medical term for a heart that beats too slowly. When your heart rate drops too low, it can't pump enough oxygen-rich blood out to the rest of your body, especially your brain.
Another major reason is heart block. Imagine a communication breakdown in your heart, where the electrical signals get delayed or completely stopped on their way from the upper chambers (atria) to the lower chambers (ventricles). A pacemaker fixes this by creating a reliable bridge, making sure the message gets through so your heart can beat in a coordinated, efficient way.
If you'd like to learn more about slow heart rhythms, our guide on what causes bradycardia is a great place to start.
The amazing thing about a pacemaker is that it does not take over your heart's job. It monitors your heart's activity and provides support only when your natural rhythm falters, making it a smart and personalized solution.
To give you a clearer picture, here are some of the most common conditions that might lead a doctor to recommend a pacemaker.
Common Reasons for a Pacemaker
Essentially, if there's an issue with the heart's electrical wiring that causes it to beat too slowly or out of sync, a pacemaker is often the most effective solution.
Different Types of Pacemakers for Different Needs
Pacemakers aren't a one-size-fits-all solution. Your doctor will choose the right type based on your specific heart condition.
Here are the main types you'll encounter:
- Single-Chamber Pacemaker: This type has one wire (called a "lead") that's placed in one chamber of the heart, usually the lower right chamber (the right ventricle).
- Dual-Chamber Pacemaker: This device uses two leads. One goes to an upper chamber (atrium) and the other to a lower chamber (ventricle), helping to coordinate the rhythm between the top and bottom of your heart.
- Biventricular Pacemaker: Also known as cardiac resynchronization therapy (CRT), this is a more advanced device with three leads. It's designed for people with severe heart failure to help both of the heart's lower chambers beat together in sync, improving the heart's pumping power.
How to Prepare for Your Pacemaker Operation
Knowing what to expect before your heart pacemaker operation can make a huge difference, helping turn that feeling of nervous uncertainty into a sense of calm and control. Let's walk through a friendly, practical checklist for the days leading up to your procedure. Our goal is to get you to the hospital feeling organized and ready.
It's completely normal to have a mix of emotions before something like this. The first step is just acknowledging them. Simple things like deep breathing exercises, or even just talking it all over with a friend or family member, can really help manage any anxiety you might be feeling.
Your Pre-Operation Checklist
A few key steps in the days before your surgery will help make sure everything goes off without a hitch. Your medical team will give you specific instructions, of course, but here are the basics you can expect.
- Medication Adjustments: Your doctor is going to want to review all your current medications. You will almost certainly be asked to stop taking certain ones, especially blood thinners, for a few days beforehand to lower the risk of bleeding.
- Fasting Instructions: You will need to stop eating and drinking for a set amount of time before the procedure. This usually starts the night before. It's a standard safety measure for any procedure that involves sedation.
- Packing Your Hospital Bag: Think comfort. Pack some loose clothing, your toiletries, and something to pass the time, like a good book or a tablet. And don't forget your phone and charger to keep in touch with everyone.
This infographic gives a great visual summary of the main prep steps.
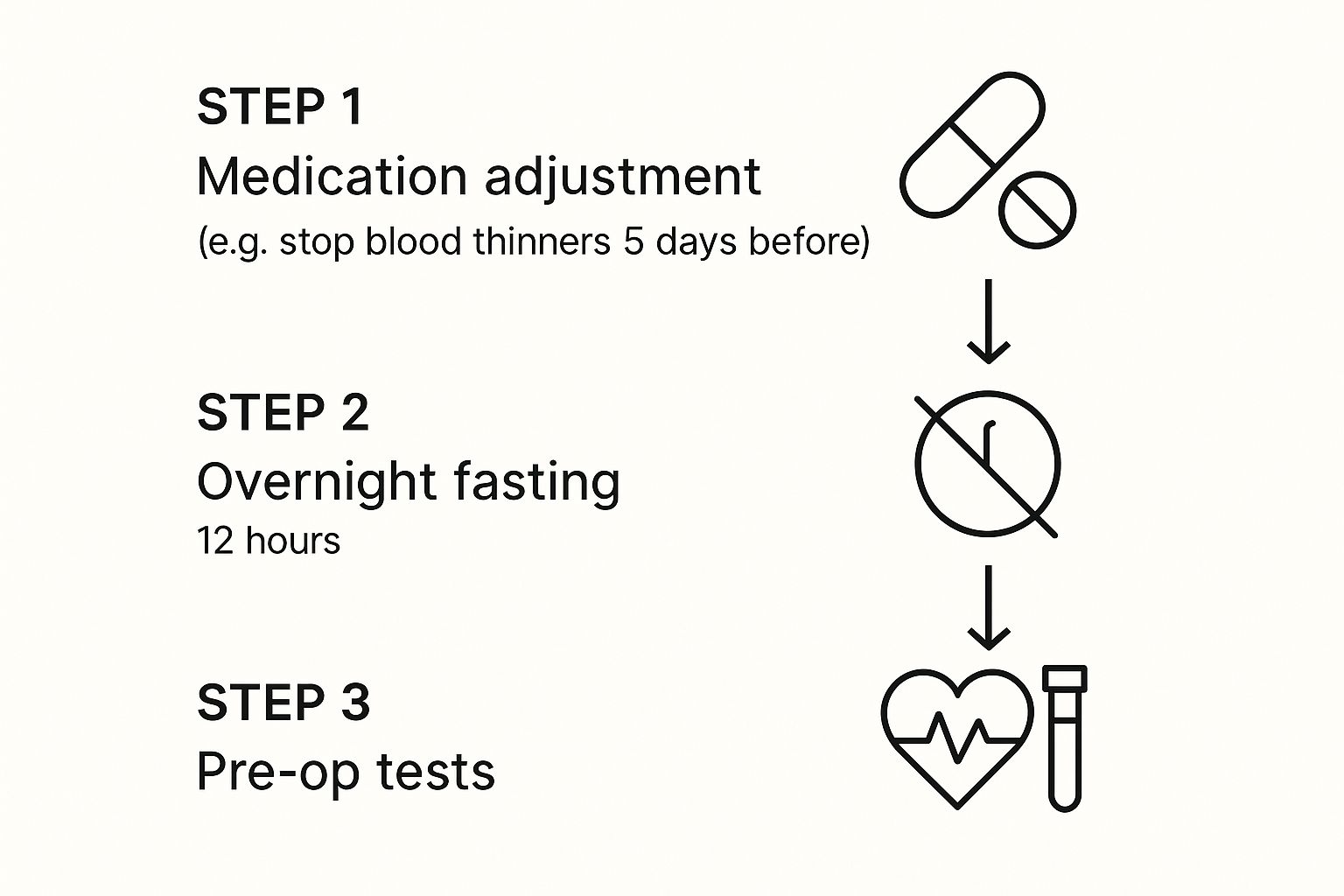
As you can see, it's really a simple sequence: tweak your meds, fast for a bit, and do some final tests to make sure you're all set.
Understanding Pre-Op Tests
Before the operation, your team will run a few quick and painless tests to get a complete, up-to-the-minute picture of your health.
An electrocardiogram (EKG) will record your heart's electrical activity, giving them a final confirmation of your baseline rhythm. You'll also likely have some routine blood work done to check things like your kidney function and blood cell counts. These tests are all about confirming that you're in the clear for a safe procedure.
Remember, every single step of this preparation is designed with your safety and comfort as the top priority. Your care team is there for you, so never hesitate to ask them anything that's on your mind.
Having a list of questions ready for your doctor can be incredibly empowering. For some great ideas, check out our guide on questions to ask your cardiologist before your appointment. Being informed is one of the best ways to feel confident about your upcoming heart pacemaker operation.
What Happens During the Pacemaker Procedure

Knowing what to expect on the day of your heart pacemaker operation can make the whole experience feel a lot less intimidating. Let's walk through the procedure step-by-step, from the moment you enter the room to the final stitch. The idea is to clear up any mystery so you feel informed and much more at ease.
First off, this is a very common and refined procedure. And while it is surgery, you'll most likely be awake the whole time. Don't worry, you won't feel any pain. You'll get a local anesthetic to completely numb the area, plus a sedative to help you feel deeply relaxed.
Step 1: Getting Started in the Procedure Room
Once you're settled, the medical team will clean the incision area, which is usually on your chest just below the collarbone. They'll cover you with sterile drapes to keep everything clean and safe. Your comfort and safety are the top priorities.
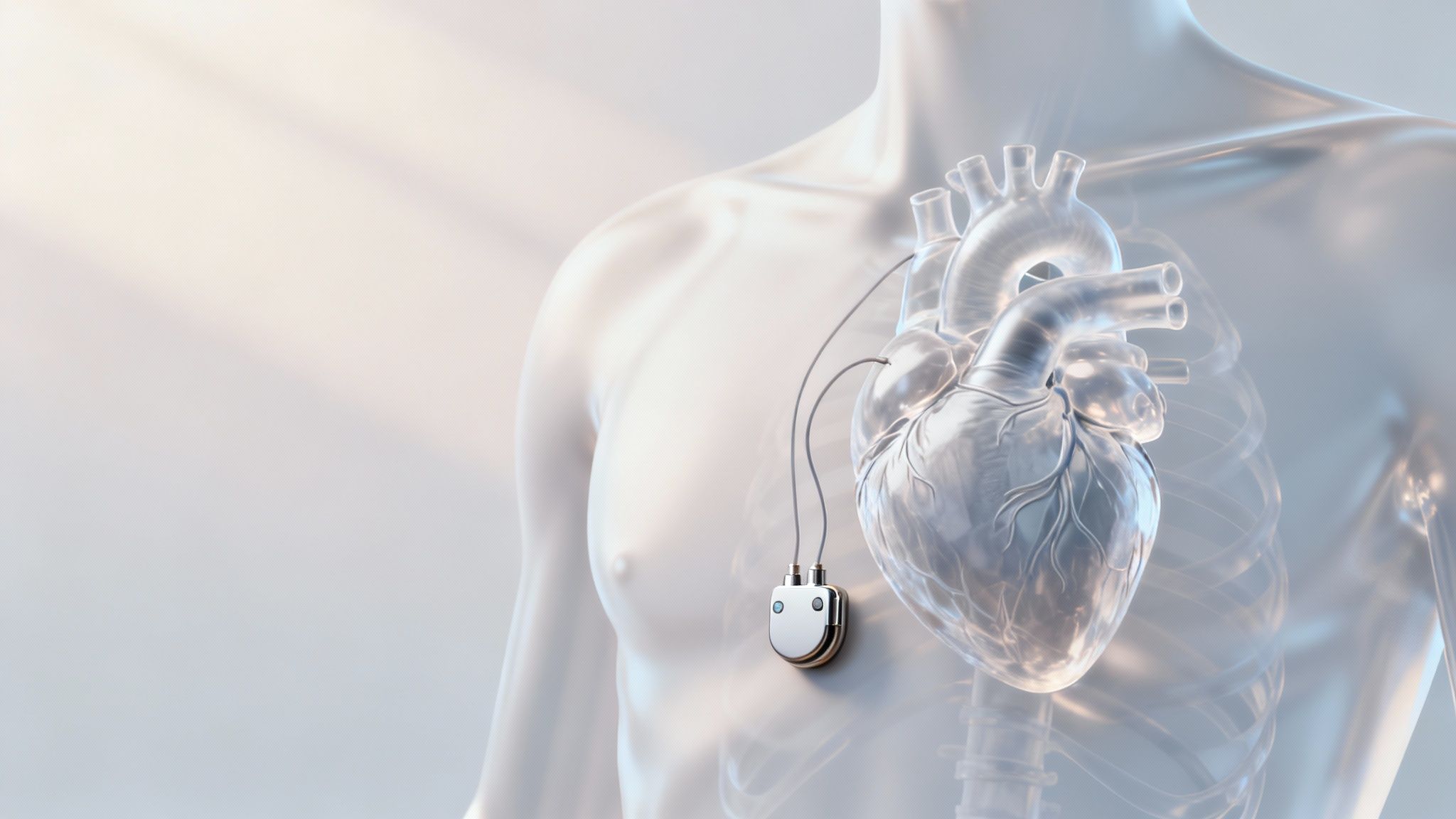
The surgeon then makes a small incision, typically about two inches long. Just beneath the skin, they create a small, neat "pocket." This is where the pacemaker device will rest securely later on.
Step 2: Placing the Pacemaker Leads
This next part is the most delicate step. The surgeon has to guide one or more thin, flexible wires, called leads, from the incision all the way into your heart.
Think of these leads as messengers. They're responsible for carrying electrical signals from the pacemaker to your heart muscle, and they also relay information about your heart's own activity back to the device.
To get them into place, the surgeon uses a large vein near your collarbone as a natural highway to your heart. With X-ray imaging as their guide, they carefully thread the leads through the vein and into the correct heart chamber. They'll then run tests to make sure the leads are in the perfect spot to communicate with your heart.
The entire heart pacemaker operation is designed to be as minimally invasive as possible. Your surgeon uses your body's own vascular system as a direct route to deliver the leads precisely where they need to go, avoiding the need for open-heart surgery.
Step 3: Connecting and Closing
With the leads perfectly positioned and tested, the surgeon connects them to the pacemaker generator, the small metal case that holds the battery and circuitry. The pacemaker is then gently tucked into that pocket they created earlier under your skin.
Finally, the surgeon closes the incision with stitches that will dissolve on their own or with a special surgical glue. A sterile dressing is placed over the site, and that's it. The whole operation usually takes about an hour from start to finish.
This amazing technology has been fine-tuned over decades. The very first clinically successful pacemaker was implanted back in 1960 by Dr. William Chardack and engineer Wilson Greatbatch, proving an internal device could safely regulate the heart. By the end of that year, nine more patients had received these early implants, with some living for more than 20 years afterward. It was this pioneering work that paved the way for the modern devices we use today. You can learn more about the incredible history of this invention.
Your Recovery and Life with a Pacemaker

With the operation complete, your focus now shifts from the procedure itself to healing and rediscovering life with a steady, reliable heartbeat. This next phase is all about giving your body the time it needs to recover and learning the simple new rhythms of life with your device. It is totally normal to feel a mix of relief and a little caution, but think of this as a brand new, positive chapter.
You can expect some soreness or discomfort around the incision for the first few days. This is a standard part of the healing process, and it is usually managed quite easily with pain medication. Your medical team’s number one priority is making sure this initial recovery period is as smooth and comfortable as possible.
The First Few Weeks
One of the most important instructions you'll get is to limit how much you move your arm on the side where the pacemaker was implanted. For a few weeks, your doctor will likely advise you to avoid lifting that arm above shoulder level or carrying anything heavy. This isn't because you're fragile; it's to give the pacemaker leads time to settle in and securely attach to your heart tissue.
Think of it like letting the roots of a newly planted tree take hold in the soil. Giving those leads some undisturbed time ensures they form a strong, lasting connection. It is a simple precaution, but it is one of the best things you can do to prevent complications and set yourself up for long-term success.
You will also get specific instructions on how to care for your incision to keep it from getting infected. This typically just means keeping the area clean and dry until it's fully healed. Your team will walk you through every step before you head home.
Returning to Your Daily Activities
As you start to heal, you will be able to ease back into your normal routine. Everyone’s timeline is a little different, but we can give you a general idea of what to expect as you get back on your feet.
Here is a general guide to what activities you can resume in the weeks following your operation.
Typical Pacemaker Recovery Timeline
Remember, this table is just a general guideline. Your doctor will provide a personalized plan based on your health and the specifics of your procedure.
Living Confidently with Your Pacemaker
Living with a pacemaker involves a few minor adjustments, but it doesn't mean restricting your life. In fact, it's quite the opposite. Most people find they can do far more than they could before the operation.
You will need to be mindful of strong magnetic fields. For example, it is a good habit to keep your cell phone at least six inches away from your device. This just means holding it to the ear on the opposite side and not carrying it in a shirt pocket. When you go through airport security, just show the staff your pacemaker ID card, and they'll guide you through an alternative screening process. It's a simple and routine part of travel.
Your pacemaker is there to empower you, not to limit you. It is a tool that helps your heart work more efficiently, giving you the freedom to live a more active and fulfilling life.
Common Questions About Pacemaker Operations
You have taken in a lot of information on this journey, and it's completely normal to still have a few questions swirling around. Getting a pacemaker is a big step, and the best way to move forward with confidence is to feel fully informed.
We've put together some of the most common questions people have about a heart pacemaker operation to give you clear, straightforward answers and a little extra peace of mind.
Will I Feel the Pacemaker Working in My Chest?
This is a really common concern, but the answer is reassuring. The vast majority of the time, you won't feel your pacemaker at all. It is designed to work quietly and seamlessly in the background, giving your heart a nudge only when it is needed.
The goal is for the device to blend into your life so well that you simply forget it is even there. This lets you get back to living with renewed energy, without having to think about the technology helping you.
How Long Does a Pacemaker Battery Last?
Pacemaker batteries are incredibly reliable and built to go the distance. On average, a pacemaker battery will last somewhere between 7 to 10 years. The exact lifespan really depends on your specific device and how often it has to step in to keep your heart in rhythm.
Your doctor will check the battery life at every single follow-up appointment, so it is not something that will ever catch you by surprise. When the battery starts getting low, it is not an emergency. You will have plenty of advance notice to schedule a simple procedure to replace the pacemaker generator, which is often a quicker process than the initial operation.
Can I Use Microwaves and Cell Phones Safely?
Yes, absolutely. This is an old myth that still hangs around, but modern pacemakers are very well-shielded against interference from everyday household electronics. Using a microwave, a computer, or watching TV poses no risk to your device.
When it comes to cell phones, a small, simple precaution is all you need. The general advice is to keep at least six inches between your phone and your pacemaker. This usually just means holding your phone to the ear on the opposite side of your body from the implant and avoiding carrying it in a shirt pocket directly over the device.
What Are the Real Risks of a Pacemaker Operation?
While any procedure carries some level of risk, pacemaker implantation is considered a very safe and routine operation. The risks are quite low. The most common issues are minor things related to the incision site, like bruising, bleeding, or a localized infection, all of which are easily treatable.
More serious complications, such as damage to a blood vessel or problems with the device leads, are much rarer.
It is helpful to remember that for the vast majority of patients, the benefits of getting a pacemaker far outweigh the small procedural risks. Studies show that only a small percentage of patients, typically around 2-5%, might need a pacemaker after other heart procedures, which really highlights how specific the need for one is.
You can also empower yourself by learning more about understanding your pacemaker ECG, which helps you take a more active role in your heart health journey.
At Qaly, we believe that understanding your heart shouldn't be a source of anxiety. Our app connects you with certified technicians who analyze your wearable ECGs in minutes, giving you the clarity and peace of mind you deserve. Take control of your heart health journey and see what makes Qaly different. Learn more at https://www.qaly.co.
On the Qaly app, human experts will interpret your ECGs for Paced Rhythm within minutes. Get started today.









.png)
.png)