Key Takeaways
Hello Heart Hero. Hearing a medical term like 'bradycardia' can feel a little scary, especially when it’s about your heart. You've come to the right place for clear, straightforward answers. We know navigating the healthcare world can feel overwhelming, and it's completely understandable to look for resources you can trust.
The short answer to what causes bradycardia is that it can come from a few different places: excellent physical fitness, the natural aging process, underlying heart conditions, or even external factors like medications.
Is a Slow Heart Rate Always Dangerous?
It's completely normal to feel a jolt of concern when you hear your heart rate is "slow." But the first thing to know is that a slow heart rate isn't automatically a sign of trouble.
For many people, especially athletes or those who are very physically active, a slower heart rate is actually a sign of a highly efficient, well-conditioned heart. Their heart is so strong that it can pump all the blood their body needs with fewer beats.
But you're here because you need more than just a simple "it depends." You're looking for real clarity, not confusing medical jargon. We get it. Trying to understand your health can sometimes feel like solving a puzzle without all the pieces, especially when you're feeling skeptical about traditional healthcare answers.
Our goal is to give you those missing pieces to replace anxiety with understanding. This guide will walk you through the causes in a way that actually makes sense, putting you back in control.
Let's break down what can cause a heart rate to slow down. Think of it like a conversation, not a lecture. We'll explore three main areas:
- Physiological Causes: These are often normal, everyday reasons, like being an athlete or even just being in a deep sleep.
- Pathological Causes: This category covers issues with the heart's own electrical system or other health conditions.
- External Factors: Things from outside the body, like certain medications or electrolyte imbalances, can also play a big role.
By looking at each of these, you can start to build a clearer picture of what might be going on. This knowledge is power - it helps you have more confident, informed conversations with your doctor and become an active partner in your own health.
.webp)
How Your Heart's Natural Pacemaker Sets the Rhythm
To really get a handle on what causes bradycardia, we first need to look at your heart’s own incredible command center. Think of it like this: your heart has its own personal drummer, a tiny but mighty cluster of cells called the sinoatrial (SA) node. This is your body's natural pacemaker, and its one job is to set the rhythm for your life.
Every single one of your heartbeats starts right here. The SA node kicks things off by generating a small electrical spark. This impulse is the signal that tells the upper chambers of your heart (the atria) to contract, pushing blood down into the lower chambers (the ventricles).
The Electrical Superhighway
Once the atria give a good squeeze, that electrical signal is on the move again. It travels to another critical relay station known as the atrioventricular (AV) node. You can think of the AV node as a smart gatekeeper. It holds onto the signal for just a fraction of a second before passing it along.
This tiny delay is absolutely crucial - it gives the ventricles just enough time to fill up with blood before they get the signal to pump. After that brief pause, the signal zips down specialized pathways to the ventricles, causing them to contract with force. That final, coordinated squeeze is what sends fresh, oxygen-rich blood out to the rest of your body.
This entire sequence, from the SA node's first spark to the ventricle's big push, creates one healthy heartbeat. It’s a beautifully efficient process that happens 60 to 100 times every minute, all without you ever having to think about it.
Any disruption along this pathway (whether due to aging, damaged tissue, or certain medications) can slow down the entire process, resulting in bradycardia.
When we discuss bradycardia, we're typically referring to an issue within the heart's electrical system. The drummer (sinus node) might be fatigued, the gatekeeper (AV node) could be too slow, or the message (electrical impulse) itself might encounter a delay as it travels along the pathway (conduction system).
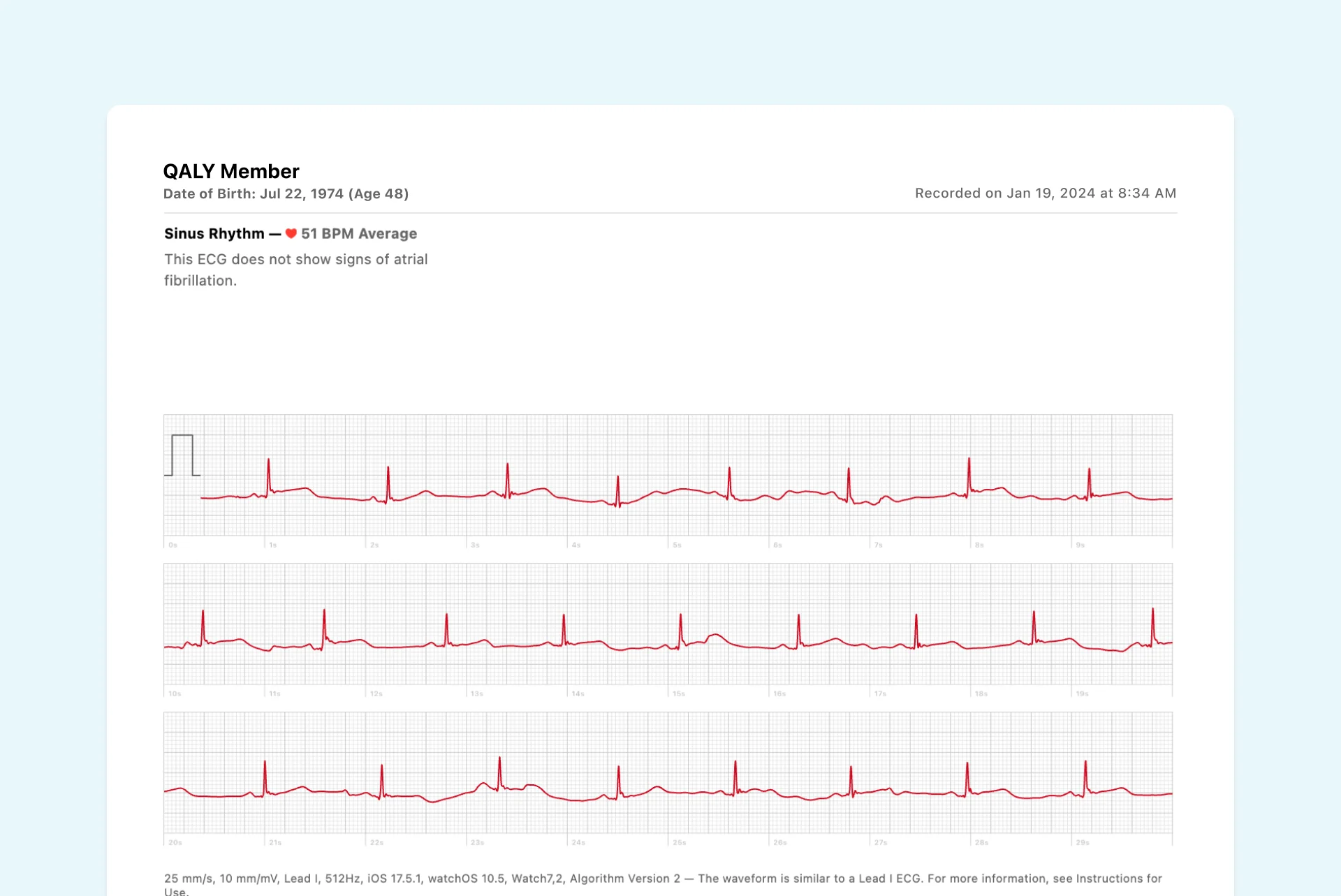
Understanding this natural rhythm is the first step. For instance, the very beginning of this electrical journey creates a specific shape on an ECG called a P wave. You can learn more about how to spot what P waves look like in your watch ECG to become more familiar with your heart's signals. By knowing how the system is supposed to work, you're better equipped to understand what happens when it slows down.

Heart-Related Causes of Bradycardia
Sometimes, the real reason behind what causes bradycardia is found right inside the heart itself. You can think of your heart’s electrical system like a tiny, intricate orchestra. If the conductor (the SA node) loses its tempo or the wiring to the musicians gets frayed, the music’s rhythm naturally slows down. This section is all about these internal, or ‘intrinsic,’ causes.
It can be confusing and a little scary when you realize your heart’s own electrical pathways are slowing things down. We’re going to walk through these reasons together, breaking them down so they’re clear and less intimidating. It's important to know that many of these issues are just a natural part of life and can be managed well.
The Natural Process of Aging
As we live our lives, our bodies change, and the heart is certainly no exception. After decades of beating faithfully, the heart's electrical wiring can start to show some natural wear and tear. This is actually one of the most common reasons for a slow heart rate in older adults.
The pathways that carry electrical signals can become slightly scarred or less flexible over time. This makes it a bit harder for those critical signals to travel as quickly and efficiently as they used to. It isn't necessarily a sign of disease, but more of a reflection of a heart that has been doing its job steadily for a lifetime.

When the Heart's Conductor Falters
Sometimes, the problem starts right at the source: the heart’s natural pacemaker, the SA node. When this "conductor" starts becoming unreliable, it leads to a condition often called sick sinus syndrome.
In this scenario, the SA node might:
- Fire too slowly: This is the most straightforward cause of bradycardia.
- Pause or skip beats: It might just fail to send out an electrical signal when it’s supposed to.
- Switch between fast and slow rhythms: This is known as tachy-brady syndrome.
Essentially, the heart's main timekeeper isn't keeping a consistent beat anymore, leading to a rhythm that is often too slow and sometimes unpredictable.
While a slow heart rate can feel isolating, bradycardia is a global health concern affecting between 0.5% and 2.0% of the general population. Advanced age is a significant factor; fibrosis and degenerative changes in the heart's electrical pathways are why approximately 75–80% of pacemaker implants are for individuals over 65.
Navigating a Roadblock in the Heart
Another common heart-related cause of bradycardia is something called heart block. Imagine the electrical signal from the SA node is a car trying to travel down a highway to the ventricles, but it suddenly hits a massive traffic jam. That roadblock is heart block.
The issue lies with the AV node - the "gatekeeper" we mentioned earlier. In heart block, the AV node either delays the signal for too long or stops some signals from getting through at all. This creates a communication breakdown between the heart's upper and lower chambers, forcing the ventricles to beat at their own, much slower, pace.
There are different degrees of heart block, from minor delays to a complete interruption of the signal. Our guide on what complete heart block looks like on your watch ECG can help you see what this specific rhythm looks like.
A slow heartbeat doesn't always point to a problem inside the heart itself. It helps to think of your body as a connected ecosystem - what happens in one area can easily ripple out and affect another. That's why a doctor looks at your whole health picture, not just your heart in isolation, when figuring out what causes bradycardia.
It can feel a little unsettling to learn that something else, like a medication you need or another health condition, could be influencing your heart’s rhythm. Let’s walk through these external factors together. Understanding these connections can be incredibly empowering and give you a much clearer view of your overall well-being.
When Medication Is the Cause
Many of us rely on medications to manage various health conditions. Sometimes, a slower heart rate isn't an unwanted side effect - it's an expected, and even desired, outcome. It’s not a mistake; it’s the medicine doing its job.
A perfect example is beta-blockers. These are often prescribed for high blood pressure or to protect the heart after a heart attack. They work by blocking the effects of adrenaline, which naturally puts the brakes on your heart rate and helps lower your blood pressure. You can dive deeper into this in our guide on how beta-blockers affect your heart and ECG.
Here's a quick look at some common external factors that can lead to a slower heartbeat.
Common External Causes of a Slow Heartbeat
It’s crucial to never stop a prescribed medication on your own, even if you suspect it's affecting your heart rate. If you’re concerned, the best first step is always a conversation with your doctor. They can determine if your heart rate is appropriate for your situation or if an adjustment is needed.
How Other Health Conditions Affect Your Heart
Beyond medications, other health issues can send signals that slow your heart's tempo. Your heart is incredibly responsive to your body's overall state, and these conditions are prime examples of that connection.
An underactive thyroid (hypothyroidism) is a classic cause. Think of your thyroid gland as your body's thermostat, regulating your metabolism. When it’s not producing enough hormones, your entire system slows down, and that includes your heart.
Another significant factor is sleep apnea, a condition where you repeatedly stop and start breathing during sleep. These pauses cause drops in blood oxygen levels, which can trigger a powerful reflex that dramatically slows the heart rate to conserve oxygen.
The causes of bradycardia are complex and can come from inside or outside the heart. External, or "extrinsic," causes are varied and can include medications like beta-blockers and calcium channel blockers, as well as health conditions like hypothyroidism and sleep apnea.
By understanding these external influences, you’re much better equipped to have a productive discussion with your healthcare provider. Knowing that your medication or another condition might be the cause provides valuable context and helps steer the conversation toward the right solution for you.
Recognizing the Warning Signs of Bradycardia
A slow heart rate can be influenced by various factors, but a number on a screen doesn't convey the complete picture. The crucial aspect to consider is how it affects your well-being. A slow heart rate isn't necessarily an issue, particularly since individuals in excellent physical condition often have a lower heart rate. Therefore, it's important to concentrate on your body's own warning signals - the symptoms that indicate when you should be more attentive.
It’s completely understandable to feel a wave of worry when you experience something unusual with your body. The goal here isn't to cause alarm but to give you a bit of reassurance and some practical guidance. Think of these symptoms as your cue to gather information for a conversation with your doctor, not as a reason to panic.
Listening to Your Body’s Signals
When your heart rate drops too low to meet your body's demands for oxygen-rich blood, it will let you know. Your brain and muscles are often the first to feel the effects of this slowdown. Becoming a better observer of these signals is the first step toward taking control.
Some of the most common warning signs include:
- Persistent Fatigue: This isn't just feeling tired after a long day. It’s a profound sense of exhaustion that doesn't seem to go away, even with plenty of rest.
- Dizziness or Lightheadedness: You might feel woozy, unsteady on your feet, or like the room is spinning. This often happens when your brain isn't getting a steady supply of oxygen.
- Shortness of Breath: Feeling breathless after minimal effort, like walking up a short flight of stairs, can be a key indicator.
- Fainting Spells (Syncope): This is the most dramatic symptom. A sudden, temporary loss of consciousness happens when the drop in blood flow to the brain is significant.
- Brain Fog or Trouble Concentrating: You might find it hard to focus or feel mentally sluggish because your brain isn't getting the fuel it needs to function at its best.
It's important to remember that context is everything. Feeling a little dizzy after standing up too quickly is very different from feeling lightheaded while sitting calmly on the couch. The persistence and circumstances of your symptoms provide crucial clues.
What These Symptoms Really Mean
Experiencing any of these signs can be unsettling, but they serve a valuable purpose. They are your body's way of communicating that something is off-balance. Rather than being a source of fear, these symptoms are powerful data points.
They transform a vague concern into concrete information you can share with your doctor. Instead of just saying, "I haven't been feeling right," you can say, "I've been feeling lightheaded and short of breath every afternoon, even when I'm just sitting and reading." This level of detail is exactly what helps create a productive partnership with your healthcare provider, ensuring you get the answers you deserve.
Taking an Active Role in Your Heart Health
When you're dealing with a health issue, especially one involving your heart, it’s easy to feel a little anxious or even powerless. The healthcare system can be confusing, and it's normal to feel like you're just along for the ride. But taking back a sense of control is a powerful first step, and today's technology gives you the tools to do just that.
You can become an active, engaged partner in your own health journey.
With at-home ECG monitoring, using your smartwatch and an app like Qaly, you can capture what's happening in the moment. Picture this: you feel a strange flutter or a brief wave of dizziness. Instead of trying to describe that fleeting sensation to your doctor weeks from now, you can take an ECG right then and there.
This simple action is a game-changer. You're no longer just a passive patient trying to recall a symptom; you're an active participant gathering concrete data. You can show your doctor exactly what your heart rhythm was doing during that episode.
Fostering a Collaborative Partnership
This shift completely changes the dynamic with your healthcare team. It becomes a real collaboration built on shared, objective information, not just your best memory of what happened. Bringing tangible ECG data to your appointments allows for much more productive conversations and helps your doctor get the full picture.
This proactive approach is about more than just data - it’s about reclaiming your peace of mind between appointments. Knowing you have a way to monitor your heart empowers you to live more confidently.
Of course, being an active participant in your health isn't just about technology. It's about a holistic approach. Embracing a healthy lifestyle also means nurturing your mental well-being; for example, exploring the mental health benefits of nature can be a wonderful part of this journey. To learn more about specific techniques for monitoring at home, check out our guide on how to check heart health at home. By combining personal monitoring with overall wellness, you build a strong foundation for managing your heart health.
When you're trying to understand your heart health, a lot of questions can pop up. That's perfectly normal. We've put together answers to some of the most common questions about what causes bradycardia to give you the clarity and peace of mind you're looking for.
Can Stress or Anxiety Cause Bradycardia?
This is a tricky one. We usually think of stress making the heart race (tachycardia), but it can have some surprising effects. A very strong reaction from your vagus nerve, which can sometimes be triggered by intense stress or sudden anxiety, can actually put the brakes on your heart rate for a short time.
However, it's important to know that ongoing, chronic stress isn't a typical cause of a persistently slow heart rate.
Is Bradycardia a Genetic Condition?
That's a fantastic question. While you don't usually inherit bradycardia itself, some of the underlying heart conditions that cause it can definitely run in families.
For instance, certain congenital heart defects or inherited problems with the heart muscle (cardiomyopathies) have a clear genetic link. If you know that heart rhythm issues are common in your family, that’s a really valuable piece of information to share with your doctor.
It's always wise to know your family's health history. For example, if close relatives needed a pacemaker at a young age, that's a significant clue that can help you be proactive about your own heart care.
How Do Diet and Exercise Affect Bradycardia?
Your lifestyle plays a massive role here. For elite athletes, a low resting heart rate is often a badge of honor - a sign of incredible cardiovascular fitness and a perfectly healthy adaptation. Their hearts are just that efficient.
On the flip side, things like a significant electrolyte imbalance can throw your heart's electrical system off. If you have very low potassium from a poor diet or dehydration, for example, it can sometimes contribute to a slow heart rate.
Wondering if it's Sinus Bradycardia? On the Qaly app, human experts will interpret your ECGs for Sinus Bradycardia within minutes. Get started today.










.png)
.png)