Key Takeaways
Hello Heart Hero. We get it. Starting a new medication like haloperidol can bring up a lot of questions, especially when you find so much conflicting information online. It’s completely normal to feel a bit cautious or even skeptical, especially when you're trying to make the best decisions for your health.
Think of this guide as a trusted partner, here to walk you through the potential haloperidol side effects in a way that's clear, supportive, and easy to understand.
Your Guide to Navigating Haloperidol Side Effects
You’re here because you want to be proactive about your health, and that’s a huge step. Taking the time to really understand your medication is one of the most powerful things you can do for yourself, especially when it feels like the healthcare system isn't always giving you the full picture.
While this guide will put a special focus on what haloperidol means for your heart, we'll also touch on the full spectrum of effects you should know about. Our goal isn't to scare you. It's to give you the knowledge you need to have better, more informed conversations with your doctor and feel confident on your health journey.
What to Expect from This Guide
We believe that clear, straightforward information is the best way to reduce anxiety. You're in the driver's seat, and we're just here to provide the map. Together, we'll break down the side effects of haloperidol, translating complex medical terms into plain language.
Here’s a look at what we’ll cover:
- Heart Health: We'll dive deep into cardiac risks, explaining what they are and why they can happen. A lot of people worry about how medications affect their heart, particularly if they already have a history of a heart rhythm disorder.
- Timelines: Knowing when side effects might show up, whether it's in the first few days or after long-term use, helps you know exactly what to look out for and when.
- Practical Steps: We'll give you real, concrete guidance on how to monitor your health, including how you can use tools you might already have to stay on top of things.
Think of this as your friendly roadmap to understanding haloperidol. We'll cut through the jargon, explain the science and the risks, and give you the tools you need to be an active participant in your own care.
By the time you finish this guide, you’ll have a much clearer picture of what to expect. This knowledge is key to working effectively with your healthcare team to make sure your treatment plan is both safe and right for you. Let's get started.
How Haloperidol Works in Your Brain
Before we get into the nuts and bolts of haloperidol side effects, it’s helpful to understand what this medication actually does. Knowing its job gives us a much clearer, more balanced picture of the whole situation. Haloperidol is what’s known as a “first-generation” or “typical” antipsychotic, and it’s been a reliable treatment for decades.
Its main purpose is to help rebalance a specific chemical messenger in your brain called dopamine. Think of dopamine as the brain's traffic controller. It helps manage your thoughts, emotions, and even physical movements. It’s a vital part of your brain's complex communication network.
Targeting Dopamine Imbalance
In conditions like schizophrenia or during an episode of acute psychosis, the brain can get flooded with too much dopamine activity. This overload can trigger symptoms that are incredibly difficult to navigate, such as:
- Hallucinations: Seeing or hearing things that aren’t really there.
- Delusions: Believing things that aren't based in reality, often with strong conviction.
- Disorganized thoughts: Struggling to connect thoughts logically or speak in a way that makes sense to others.
Haloperidol works by blocking some of the dopamine receptors in the brain. Imagine your brain has countless tiny "docks" (the receptors) where dopamine "ships" land to deliver their messages. Haloperidol acts like a temporary gatekeeper, blocking some of these docks. This reduces the overall traffic of dopamine signals, which helps ease the symptoms and bring back a sense of stability.
By dialing down the excess dopamine messages, haloperidol can bring significant relief and clarity. It's a powerful tool, often used when other treatments haven't quite done the job.
This mechanism is the key to its effectiveness, but it also explains why some side effects can pop up. The very action that calms psychiatric symptoms can also throw a wrench into other bodily functions that rely on dopamine, like controlling movement and regulating hormones.
Understanding this trade-off is the first step. The goal of treatment is never just about stopping symptoms. It's about partnering with your doctor to find a dose that gives you the most benefit with the fewest downsides. This context is crucial as we start to explore the potential physical and cardiac effects in the next sections.
Understanding Common Movement-Related Side Effects
While haloperidol is working to calm your thoughts and emotions, its impact on dopamine can sometimes spill over into the part of your brain that coordinates movement. It can be unsettling to notice your body moving in ways you don't intend, but knowing what to look for is the first and most important step.
These movement changes are known in the medical world as extrapyramidal symptoms (EPS). You can think of it like this: the same chemical action that turns down the volume on psychiatric symptoms can also muffle the signals your brain sends to your muscles. It's a direct, and often predictable, effect of how the medication works.
It's important to know that you're not alone if this happens, and these are symptoms your doctor is very familiar with managing. The key is always to listen to your body and talk openly with your healthcare team about what you're feeling.
Symptoms That Can Appear Sooner
Some movement side effects can show up pretty quickly after starting haloperidol, sometimes within the first few days or weeks. This group of symptoms is often called parkinsonism because they can look a lot like the symptoms of Parkinson's disease.
You might notice things like:
- Stiffness or Rigidity: Your muscles might feel tight and less flexible, making movements feel wooden or difficult. This is often noticeable in the arms, legs, or neck.
- Tremors: A slight shaking, usually in the hands, that’s most obvious when you’re resting.
- Slowed Movement: It might feel like simple actions, such as getting out of a chair or walking across a room, take much more effort and happen more slowly. This is called bradykinesia.
- Restlessness: A powerful inner feeling that you have to be moving. This can look like pacing, fidgeting, or just being unable to sit still. This specific symptom is called akathisia.
These early symptoms are usually tied to your dose. That means they can often be improved by adjusting your medication, so it's critical to tell your doctor right away instead of waiting for them to get better on their own.
The Long-Term Risk: Tardive Dyskinesia
There’s another type of movement side effect to be aware of, called tardive dyskinesia (TD). This one is a more serious concern linked to taking haloperidol for a long time, typically after months or even years of treatment.
Tardive dyskinesia involves involuntary, repetitive body movements. The risk goes up the longer you're on the medication and is also higher for older adults.
The most common signs of TD involve the face and mouth, such as:
- Lip smacking, puckering, or pursing
- Tongue thrusting or sticking the tongue out
- Rapid, uncontrolled blinking
- Chewing or grimacing motions
In some cases, TD can also cause jerky or writhing movements in the arms, legs, or torso. This is one of the most serious haloperidol side effects because, in some cases, the movements can become permanent, even after the medication is stopped. This is precisely why regular check-ins with your doctor are so important.
Since these movement-related side effects can seriously affect your stability, especially in older populations, learning about specific balance assessment tests for elderly patients can be helpful. Clinical studies show parkinsonism usually appears within days to months of starting haloperidol, while tardive dyskinesia tends to emerge after months to years of use. You can explore more about these timelines by reading the research on these side effect patterns.
Haloperidol and Your Heart's Electrical Rhythm
Let's shift our focus to the heart. We know this topic can feel sensitive and bring up a lot of anxiety, and it's completely understandable to be concerned about how any medication might affect such a vital part of your health. Our goal here is to talk about this openly, to demystify one of the more serious potential haloperidol side effects and empower you, not alarm you.
Haloperidol has the potential to affect your heart’s electrical system. You can think of your heartbeat as a perfectly timed piece of music, with each part of the beat happening in a precise sequence. There's a specific part of this rhythm, which we can measure on an ECG, called the QT interval.
This interval represents the time it takes for your heart's lower chambers, the ventricles, to squeeze blood out and then fully reset for the next beat. Haloperidol can sometimes cause this resetting phase to take a little longer than it should.
What Is QTc Prolongation?
When the QT interval stretches out and becomes too long, it’s a condition known as QTc prolongation. The "c" just means the measurement has been "corrected" for your heart rate, giving us a more standardized number to work with.
Imagine a musician holding a single note for too long in the middle of a song. That one prolonged note could throw off the entire rhythm, making the music unstable and unpredictable. In a similar way, a prolonged QTc interval can make the heart's electrical system vulnerable to a rare but very serious type of irregular heartbeat.

This is why cardiac toxicity, specifically QT interval prolongation, is a well-documented risk with haloperidol. It's a particular concern with higher-than-recommended doses or when the medication is given intravenously. You can discover more insights about this risk and the data that supports it in drug safety references.
The key takeaway is this: A longer QT interval doesn't automatically mean something dangerous will happen, but it does increase the risk. This is why careful monitoring by your healthcare team is so important. They are there to watch for these changes and keep you safe.
This infographic helps visualize some of the other effects haloperidol can have on the body, particularly those related to movement.
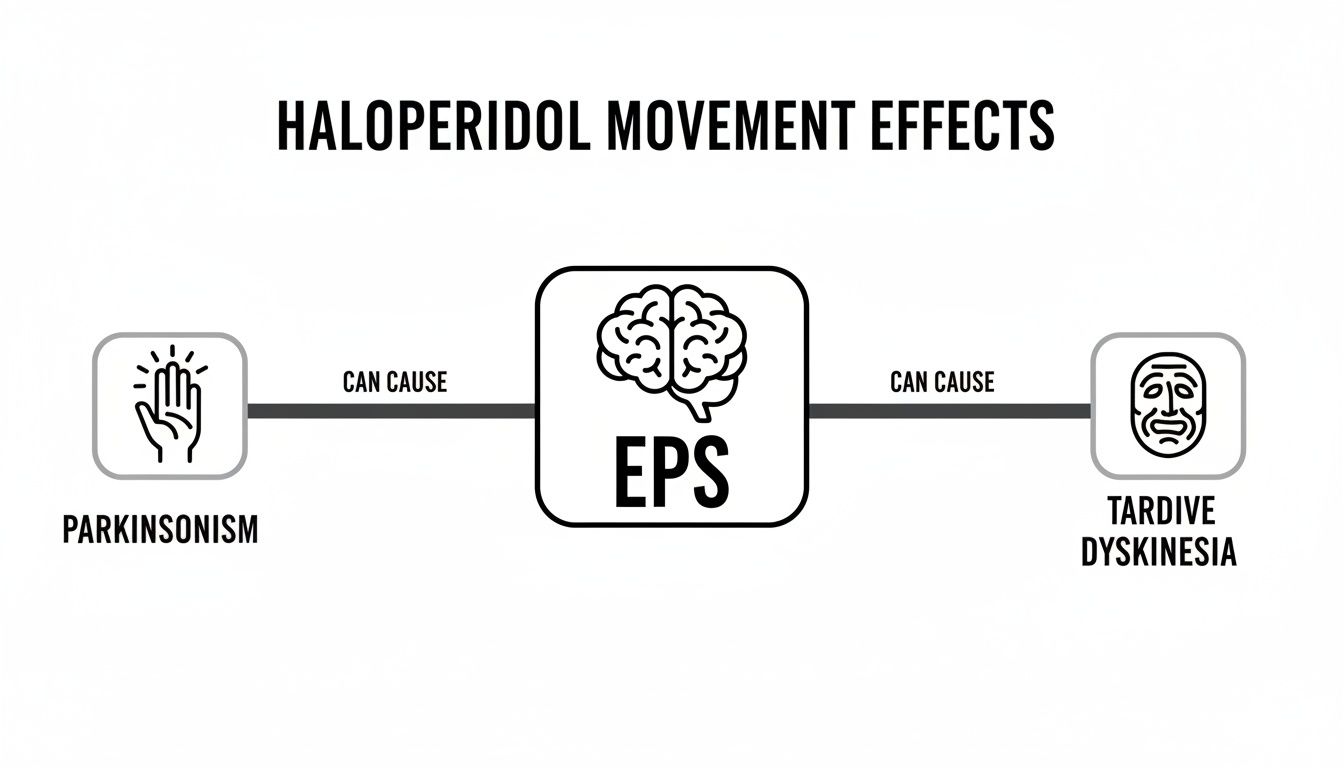
As you can see, the image highlights how extrapyramidal symptoms (EPS) are a central effect, which can then branch out into issues like Parkinsonism and Tardive Dyskinesia.
Why Careful Monitoring Is Essential
Because of this potential effect on your heart, your doctor will likely take some precautions. It's standard practice for them to be thorough and proactive.
Here’s what that might look like:
- Baseline ECG: Your doctor may order an ECG (also called an EKG) before you even start taking haloperidol. This gives them a clear picture of your heart's natural rhythm and your baseline QT interval.
- Follow-Up ECGs: They will also likely schedule periodic ECGs while you are on the medication. This allows them to see if there are any changes over time and to catch any QTc prolongation early on.
- Electrolyte Checks: Levels of certain minerals in your blood, like potassium and magnesium, play a huge role in maintaining a steady heart rhythm. Your doctor may order blood tests to make sure these are in a healthy range.
It's also worth noting that other medications can affect the QT interval. This is why it’s so important to tell your doctor about everything you take, including other prescriptions, over-the-counter drugs, and supplements. Some combinations, like certain blood thinners, require careful management. For example, if you are also taking anticoagulants, you might find it useful to learn more about the different types like Xa factor inhibitors and how they work.
This isn’t about creating fear. It’s about highlighting the importance of a strong partnership with your doctor. They have the expertise to weigh the benefits of haloperidol against these risks and to monitor you closely. Your role is to be an active, informed participant by attending your appointments and communicating openly about how you feel.
Identifying Your Personal Risk Factors
When it comes to haloperidol side effects, it's never a one-size-fits-all situation. Your unique body, health history, and even your lifestyle all come into play. Think of it less like a standard warning label and more like a personalized puzzle that you and your doctor are solving together.
It's completely understandable to feel skeptical or overwhelmed by the healthcare system sometimes. Taking the time to understand your own risk factors is one of the most powerful things you can do. It equips you to be your own best advocate, ask the right questions, and truly partner with your doctor on your care plan.
Heart-Related Risk Factors to Consider
As we've touched on, haloperidol can tweak the heart's electrical rhythm. Certain pre-existing conditions or imbalances can make this side effect more likely, which is why being completely open with your doctor is not just helpful, it's essential for your safety.
Here are some key factors that can increase the risk of cardiac side effects:
- A History of Heart Problems: If you already have a known heart condition, especially something involving an irregular heartbeat or a history of a slow heart rate (bradycardia), your heart might be more sensitive to haloperidol's effects.
- Low Electrolyte Levels: Your heart’s electrical system runs on a delicate balance of minerals like potassium and magnesium. When these levels are low, something that can happen due to other health issues or medications, it dials up the risk of QTc prolongation.
- Other Medications: You'd be surprised how many common medications can also affect the QT interval. This list includes certain antibiotics, antidepressants, and other antipsychotics. It's critical to make a complete list of everything you take, including over-the-counter drugs and supplements, for your doctor.
Your personal medical history is the most important piece of this puzzle. By sharing every detail with your doctor, you’re giving them the full picture they need to make the safest and most effective decisions for your care.
It's also a great idea to have a clear understanding of your overall heart health. You can learn more about how doctors evaluate these factors by reading our guide on calculating your risk score for cardiovascular disease.
Risk Factors for Movement-Related Side Effects
Just like with the heart effects, certain factors can make you more susceptible to the movement-related side effects of haloperidol, such as parkinsonism or tardive dyskinesia. Your doctor will weigh these carefully when deciding on the right dose and how to monitor you.
The primary risk factors for these symptoms include:
- Age: Older adults are often more sensitive to medications across the board, and they face a higher risk of developing both early movement symptoms and long-term tardive dyskinesia.
- Dose and Duration: This one is pretty straightforward. Higher doses of haloperidol and longer-term treatment significantly increase the risk. This is exactly why doctors aim to use the lowest effective dose for the shortest time necessary.
- Genetics: Some emerging research suggests your genetic makeup might play a role in how susceptible you are to movement disorders, though this is still an active area of study.
It's also helpful to understand how these risks look in broader studies. For instance, one large-scale analysis of antipsychotic users found some significant differences in health outcomes. The study reported that the mortality rate for haloperidol users was 186.8 deaths per 1,000 person-years, a number that was substantially higher than for some other medications. You can read the full research about these mortality rate findings on PubMed. Doctors use data like this not to scare patients, but to carefully weigh the benefits against the risks for each individual, ensuring the treatment choice is the right one for your specific situation.
Practical Ways to Monitor Your Heart Health
Taking an active role in your health can be incredibly empowering, especially when dealing with the complexities of the healthcare system. Modern technology has given us more tools than ever to become true partners in our own care. Let's walk through some practical ways you can keep an eye on your heart health while taking haloperidol, turning any concerns into a productive conversation with your doctor.

This journey always starts with the fundamentals: regular check-ups and the ECGs your doctor orders. These clinical tests provide the baseline data your healthcare team needs to make sure your treatment is both safe and effective. They're the gold standard for a reason.
But your involvement doesn't have to stop when you leave the clinic. Personal ECG devices, like those built into many popular smartwatches, can be an incredibly valuable addition to your health toolkit.
Using Personal ECG Devices as a Tool
Let's be crystal clear about one thing: a smartwatch ECG is not a substitute for a doctor's diagnosis or a formal 12-lead ECG from a clinic. Think of it instead as a way to gather more data points over time. It helps you keep tabs on your heart's rhythm during your day-to-day life, in between your scheduled appointments.
These devices can spot certain irregularities and even measure things like your QTc interval, which is especially important when we're talking about haloperidol side effects. By taking readings at different times of the day, you can begin to build a clearer picture of what’s normal for you.
This isn’t about self-diagnosis. It’s about collecting personal health data so you can have a more informed, detailed conversation with your doctor. You’re bringing more to the table.
If you want to get a better handle on what that QTc measurement actually means, our guide on whether you should be worried about a long or short QTc interval breaks it down further. Understanding the "why" behind the numbers can make your monitoring feel much more empowering.
Making Sense of Your Wearable ECG Data
Okay, so you’ve taken an ECG on your watch. Now what? That squiggly line on your screen can look pretty intimidating, but that's exactly where services like Qaly come in.
Qaly connects you with certified technicians who can read your wearable ECG recordings, often in just a few minutes. This kind of service can help you by:
- Providing Peace of Mind: Getting a professional set of eyes on an unusual reading can go a long way in reducing anxiety.
- Spotting Potential Issues: Technicians can identify over 30 types of arrhythmias and other irregularities that you can then bring to your doctor's attention.
- Tracking Trends Over Time: By having your ECGs reviewed regularly, you can monitor for any changes in your QTc interval or other heart metrics.
This information allows you to walk into your next appointment with a detailed report. Instead of just saying, "I felt a little funny last Tuesday," you can show them specific, analyzed data. That makes for a much more effective discussion about your health. For those looking for even more connected care, exploring options like remote patient monitoring can offer more ways to stay in sync with your healthcare team.
Ultimately, monitoring is all about being an informed, active participant in your own care. When you combine your doctor’s expertise with the data you've gathered, you create a powerful partnership focused on one thing: keeping you safe and healthy.
Common Questions About Haloperidol Side Effects
Trying to understand a new medication can feel like assembling a puzzle with a few pieces missing. It’s natural to have questions, and getting straight answers is the first step toward feeling confident about your health. We've put together some of the most common questions about haloperidol side effects to give you that clarity.
It’s all too easy to get tangled up in medical terms or feel like your worries aren’t being heard. This is where we break things down, tackling your questions directly so you feel more informed and prepared.
How Long Does It Take for Side Effects to Appear?
The timing of side effects can really vary, which is why having a rough timeline is so helpful. Some effects pop up almost immediately, while others are tied to using the medication over a longer period.
Here are the different timelines:
- Within Hours to Days: You might notice things like drowsiness, dizziness, or a dry mouth pretty quickly after starting haloperidol. On the flip side, feelings of agitation and anxiety can also start to ease within just a few hours.
- Within Days to Weeks: This is often when early movement-related symptoms, like muscle stiffness or tremors (known as parkinsonism), can show up as your body gets used to the medication.
- After Months or Years: The most significant movement disorder, tardive dyskinesia (involuntary movements, often in the face), is a long-term risk. It usually appears after being on the treatment for an extended time, which is why your doctor will want to monitor you closely over the long haul.
Knowing this timeline isn't about bracing for impact. It's about being aware of what to look for and when, so you can have productive conversations with your doctor right from the start.
Being mindful of these windows allows you and your healthcare team to be proactive, making any necessary adjustments to keep your treatment as safe and effective as possible.
Are Haloperidol Side Effects Permanent?
This is a big one, and a question we hear all the time. The answer really hinges on the specific side effect.
Many of the more immediate effects, like drowsiness, dizziness, or even those early parkinsonism symptoms, are typically reversible. They often get better or disappear entirely if the dose is lowered or if the medication is stopped (always under a doctor's supervision, of course).
However, the main concern when it comes to permanence is with tardive dyskinesia (TD). This condition, which involves involuntary movements, can become permanent for some people, even after they've stopped taking haloperidol. This is precisely why your doctor will schedule regular check-ups: to screen for any early signs of TD. Catching it early is key to managing it effectively.
What Should You Do If You Experience a Side Effect?
If you start noticing any new or worrying symptoms after starting haloperidol, the single most important thing you can do is talk to your doctor right away. Never stop taking your medication suddenly on your own, as that can create a whole new set of problems.
Your doctor is your partner in this. They can help you figure out if what you're feeling is a side effect and then map out the best path forward. That might mean:
- Adjusting your dose.
- Adding another medication to help manage the side effect.
- Switching to a different antipsychotic medication entirely.
When it comes to heart-related symptoms, like a racing heartbeat, feeling faint, or severe dizziness, you should get medical help immediately. These can be red flags for a more serious issue that needs to be checked out right away. Remember, you know your body best, and your input is a vital part of your care.
Qaly gives you the power to monitor your heart health from your wrist, providing expert analysis of your wearable ECGs in minutes










.png)
.png)