Key Takeaways
If you or a loved one has a pacemaker, understanding its function and how it appears on an ECG is a crucial part of managing heart health. A pacemaker is a small device implanted under the skin, usually near the collarbone, that sends electrical pulses to the heart to help it beat at a normal rate and rhythm.
Why Pacemakers Are Implanted
Pacemakers are typically implanted to treat bradycardia (a heart rate that is too slow) or certain types of heart block, where the heart’s natural electrical signals are disrupted. They ensure that your heart beats effectively, preventing symptoms like dizziness, fatigue, and fainting. Modern pacemakers are highly sophisticated, capable of sensing your heart’s natural rhythm and only pacing when necessary.
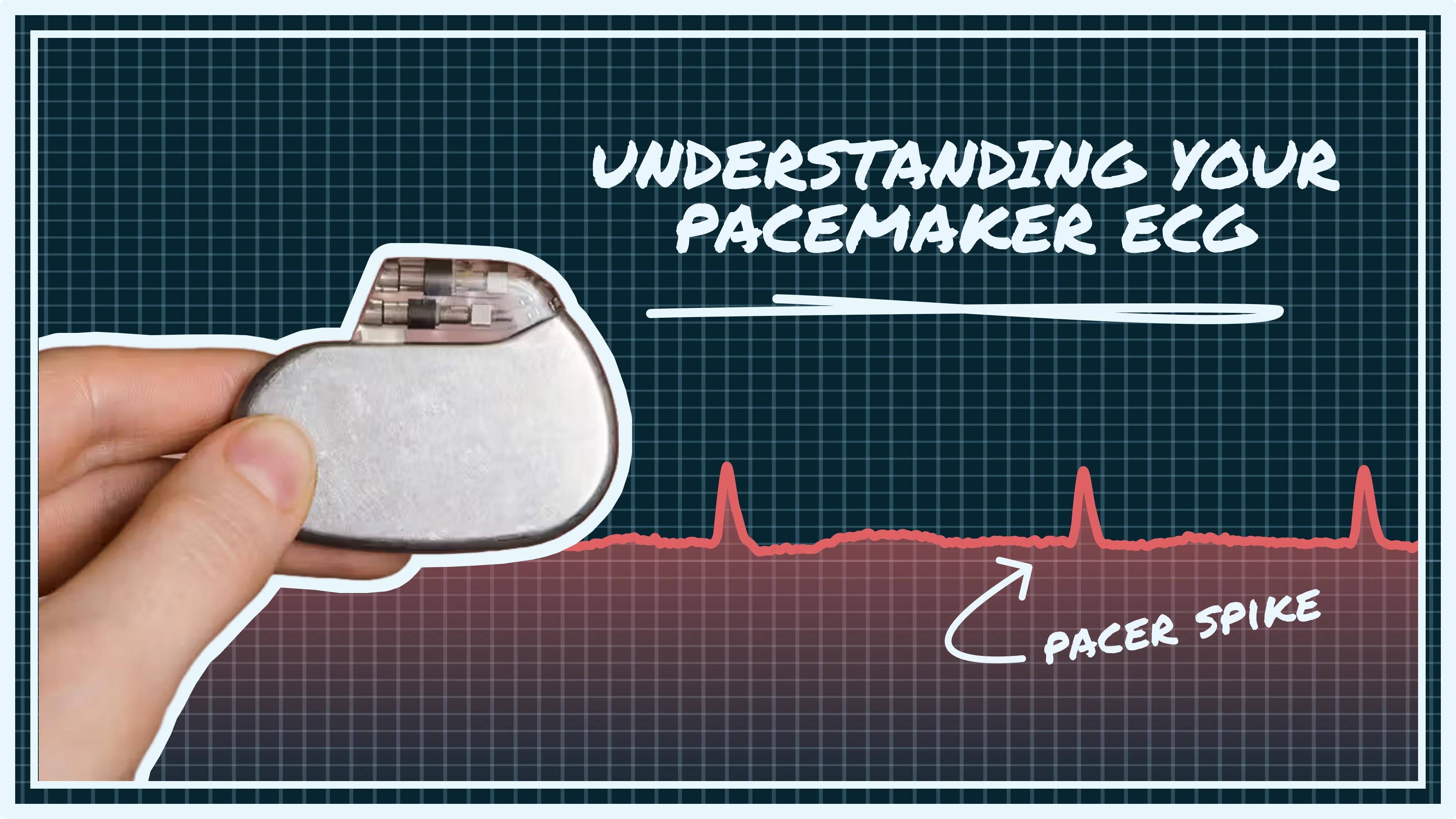
How Pacemakers Appear on an ECG
On an ECG, a pacemaker’s activity is visible as distinct spikes, known as pacing spikes, immediately followed by a QRS complex. These spikes indicate that the pacemaker has delivered an electrical impulse to stimulate a heartbeat. The appearance of the QRS complex after a pacing spike can vary depending on where the pacemaker lead is placed in the heart.
.webp)
For example, if the pacemaker lead is in the right ventricle, the paced QRS complex will often appear wide and resemble a left bundle branch block pattern. If the lead is in the right atrium, you will see a pacing spike before the P wave. Dual-chamber pacemakers, which pace both the atrium and ventricle, will show two pacing spikes – one before the P wave and one before the QRS complex.
Paced Beats vs. Intrinsic Beats
It’s important to differentiate between paced beats and intrinsic beats. An intrinsic beat is a heartbeat generated by your heart’s natural electrical system, without assistance from the pacemaker. A well-functioning pacemaker should only pace when your heart’s natural rhythm falls below a programmed rate or when there’s a block in the natural conduction pathway. This is known as demand pacing.
Sensing and Timing in Pacemakers
Modern pacemakers are designed to be highly adaptive. They can sense your heart’s own electrical activity and only deliver a pulse when needed. This sensing function is crucial for preventing competition between the pacemaker and your natural heart rhythm. If the pacemaker fails to sense an intrinsic beat, it might deliver a pulse inappropriately, which can sometimes be seen on an ECG as a pacing spike that falls within or too close to a natural QRS complex.
Recognizing Pacemaker Malfunctions on ECG
While pacemakers are generally very reliable, there are certain ECG patterns that might indicate a problem and warrant medical attention.
- Failure to capture: The pacemaker delivers a pacing spike, but it’s not followed by a QRS complex. This could be due to lead displacement, battery depletion, or an increase in the heart’s pacing threshold.
- Failure to sense: The pacemaker fails to detect your heart’s natural beats. This can lead to the pacemaker firing inappropriately, even when your heart is beating on its own. On an ECG, this would appear as pacing spikes occurring too frequently or at fixed intervals, without regard for your intrinsic rhythm.
- Oversensing: The pacemaker mistakenly interprets non-cardiac signals (like muscle movements or electrical interference) as heartbeats and inhibits pacing when it should be firing. This can lead to pauses in your heart rhythm.
- Undersensing: The pacemaker doesn’t detect your heart’s own beats, leading to unnecessary pacing.
Changes in the appearance of the paced QRS complex, or a sudden change in your heart rate or rhythm, should also be reported to your healthcare provider. These could indicate lead issues, battery problems, or changes in your underlying heart condition.
Follow-Up and Monitoring
If you have a pacemaker, regular follow-up appointments with your cardiologist are essential. During these appointments, your pacemaker will be interrogated using a special device that can read its settings, battery life, and how well it’s functioning. This allows your doctor to make adjustments to optimize your pacemaker’s performance.
Your cardiologist will also review your ECGs, both those taken in the clinic and any recordings from your home monitoring device or smartwatch. They will look for any signs of pacemaker malfunction, such as failure to capture or sense, and assess how well your pacemaker is supporting your heart rhythm.
Smartwatches as a Tool for Pacemaker Users
Smartwatches with ECG capabilities are becoming an increasingly powerful tool for people with pacemakers. While they are not a replacement for a 12-lead ECG or a pacemaker interrogation, they provide accessible, real-time insights into your heart rhythm and rate.
Smartwatch ECGs can help detect:
- Consistently slow heart rates (below your pacemaker’s programmed minimum rate)
- Irregular rhythms that may not be paced appropriately
- Sudden rate changes or pauses that could signal a sensing or capture issue
These recordings, when shared with your cardiologist, can assist in early identification of potential pacemaker issues and help guide timely follow-up or device reprogramming.
Thanks to advances in smartwatch technology, many models now allow you to store, view, and share your ECGs directly from your phone. Some also allow trend tracking over time, which can reveal subtle changes in your heart’s behavior even before symptoms arise.
Smartwatches vs. Clinical ECGs
While smartwatch ECGs are typically single-lead, they can still reveal meaningful patterns—especially if you know what to look for. Though they may not always display pacing spikes clearly, frequent recordings can still flag issues like:
- Missed beats
- Unexpected pauses
- Inappropriate bradycardia or tachycardia
They are best viewed as a daily window into your cardiac rhythm, serving as an early-warning system that complements your clinical care. With guidance from your provider, your smartwatch can be a practical, proactive addition to your heart health toolkit.
Listening to Your Body
Living with a pacemaker means learning to listen to your body and understanding the signals your heart and device are sending. While the technology is advanced, your active participation in monitoring your health is key. Pay attention to any new or worsening symptoms, such as dizziness, fainting, shortness of breath, or persistent fatigue, as these could indicate a pacemaker issue.
Understand your pacemaker’s basic settings, such as its lower rate limit, and be aware of what your normal heart rate should be. If you feel your heart rate is consistently below this limit, or if you experience palpitations or irregular beats, contact your healthcare provider.
Keep a record of your symptoms and any unusual ECG readings from your smartwatch. This information can be invaluable for your cardiologist during follow-up appointments. Avoid strong magnetic fields or certain electrical devices that could interfere with your pacemaker, and always inform medical professionals that you have a pacemaker before any procedures.
Conclusion
That brings us to the end of our guide on understanding your pacemaker ECG and knowing what to look out for. We hope it gave you more clarity and confidence when reviewing your heart data.
If you’re still unsure about what your ECGs mean, you’re not alone. We know it can be stressful and confusing to deal with irregular rhythms, especially with a pacemaker. That’s why we built the Qaly app — to support you and the millions of others navigating heart rhythm issues. On Qaly, real human experts interpret your smartwatch ECGs in minutes, giving you peace of mind when you need it most.
To get started, download the Qaly app from the App Store or Play Store. And if you ever have questions or need assistance, reach out to us anytime at support@qaly.co.
From all of us at Qaly, stay heart healthy ❤️
Not sure what your ECG means? Qaly experts review your smartwatch ECGs in minutes. Get clarity today.









.png)
.png)