Key Takeaways
Hello, heart hero.
The road to recovery after a heart attack can feel like staring into a great unknown. People often wonder how long it will take to feel "normal" again. While every journey is different, recovery generally happens in stages, moving from a few days in the hospital to several months of healing and lifestyle changes.
Most people start feeling strong and confident in their new normal within two to three months, but your personal timeline will depend on a whole host of factors.
Your Recovery Journey Begins Now

We get it, this is an overwhelming time, and we're here to walk this path with you. After something as life-changing as a heart attack, it's completely normal to be riding a rollercoaster of emotions, from fear and confusion to relief and gratitude.
Think of this guide as your trusted companion, a roadmap designed to make the heart attack recovery timeline a lot less mysterious. You're probably tired of one-size-fits-all medical advice that doesn't feel like it applies to you. You're looking for real answers, not just textbook definitions.
A Roadmap for Your Unique Path
Our goal is to give you a clear, empathetic guide that puts knowledge in your hands. This isn't a rigid set of rules, but more like a map that points out the common landmarks on the road to getting better. Your journey will have its own pace and its own detours, and that's perfectly okay.
We'll break down each stage, from those critical first hours in the hospital to the months ahead as you build a new, stronger normal. This isn't a lecture; it's a conversation about what to expect.
We will cover:
- Medical Milestones: Making sense of the procedures and medications that are key to your initial healing.
- The Emotional Journey: Acknowledging the psychological side of things and finding healthy ways to cope.
- Practical Lifestyle Shifts: Building new habits that will protect your heart for the long haul.
Your path forward is unique, but you are not alone on this journey. Millions of people have successfully navigated their recovery, and their experiences help light the way for others.
Taking Control of Your Health Story
Facing recovery can make you feel like you’ve lost the steering wheel. The healthcare system can be confusing, and it's easy to feel like a passenger in your own health story. This guide is designed to put you back in the driver's seat.
By understanding the "why" behind each step, why rest is so crucial in week one, why cardiac rehab is a game-changer, and why small dietary changes make a huge impact, you become an active partner in your own care.
You'll learn what questions to ask your doctors and how to listen to your body's signals. This knowledge is your greatest tool for reclaiming your life with confidence and building a resilient, heart-healthy future. Let’s begin this journey together.
The First 72 Hours: In The Hospital
The first few days after a heart attack are, without a doubt, the most critical part of your entire recovery. Think of this time as an emergency pit stop for your heart - it's a period for immediate repairs and stabilization. You’re in a safe, controlled environment where the only thing that matters is getting your heart stable and preventing any more damage.
It's completely normal to feel overwhelmed, confused, or even a bit out of it during these first hours. You’ve just been through a massive physical and emotional event, and your body and mind are working overtime to process it all. The intensive care you're receiving is the first and most important step toward getting you back on your feet.
Restoring Blood Flow to Your Heart
Right now, the number one goal is to get blood flowing back to your heart muscle. A heart attack is essentially a plumbing problem, a blockage, like a major traffic jam in an artery, has cut off blood flow to a part of your heart. The medical team's top priority is to clear that jam, and fast.
You’ll probably hear them discussing a few different procedures. Let’s break down the most common ones in simple terms.
One of the most effective is called percutaneous coronary intervention (PCI), but you'll more likely hear it called angioplasty. It's a non-surgical procedure where doctors guide a very thin tube with a tiny balloon on its tip through a blood vessel up to the blocked artery. Once in place, they inflate the balloon to flatten the plaque against the artery wall and often place a small mesh tube called a stent to act as a scaffold, keeping the artery propped open.
The widespread use of PCI has been a game-changer for heart attack survivors. To give you an idea, the rate of in-hospital heart failure after a heart attack plummeted from 46% in 1996 to just 28% by 2008, a huge improvement credited largely to how effective PCI is at saving heart muscle.
Constant and Careful Monitoring
For these first 72 hours, you'll be hooked up to monitors that seem to beep and flash nonstop. We know it can feel a little unnerving, but it’s a very good thing. It means a dedicated team is keeping a close, constant watch over you.
They are tracking several key vitals:
- Heart Rhythm: An electrocardiogram (ECG or EKG) will be running continuously to make sure your heart is beating in a steady, regular pattern. This helps them spot any potential irregularities right away.
- Blood Pressure: Keeping your blood pressure in a safe zone is crucial. It reduces the strain on your healing heart.
- Oxygen Levels: That little clip on your finger is a pulse oximeter, and it’s making sure your blood is carrying plenty of oxygen.
This round-the-clock monitoring allows your care team to make real-time adjustments to your treatment, keeping your recovery on the right path. After a heart attack, the heart's electrical system can be a bit unstable, so watching for abnormal rhythms is a top priority. To get a better handle on what your doctors are looking for, you can learn more about heart arrhythmia symptoms in our guide.
The Role of Essential Medications
You'll almost certainly be started on several new medications immediately. It can feel like a lot to keep track of, but every single one has a specific job to do in protecting your heart.
Think of these medications as your personal support crew, working behind the scenes to help your heart heal and prevent future problems. They are a cornerstone of your long-term wellness plan.
Here are a few of the common medications you might receive:
- Blood Thinners (like aspirin or clopidogrel): These make your blood less "sticky," which is vital for preventing new clots from forming, especially around a new stent.
- Beta-Blockers: These help slow your heart rate and lower your blood pressure. This gives your heart a much-needed break by reducing its workload, allowing it to heal more effectively.
- Statins: These are prescribed to lower your "bad" cholesterol (LDL). This not only helps prevent new blockages but also helps stabilize the plaque that's already in your arteries.
Your medical team will walk you through what each medication does and why it's so important for you. Never hesitate to ask questions; understanding your treatment is an empowering part of taking control of your recovery.
Navigating The First Month At Home
Coming home from the hospital is a huge milestone on your recovery journey. It’s a moment of relief, a return to the familiar, but let’s be honest, it can also feel a little daunting. The safety net of 24/7 medical care is gone, and you're suddenly the one in charge.
Feeling this way is completely normal. The first month back home is a delicate dance between resting your body and slowly, carefully, re-engaging with your life. Your body is doing some incredible repair work behind the scenes, and your main job is to give it the right environment to heal.
Understanding Your Heart’s Healing Process
Think of your heart muscle like a badly sprained ankle. After the initial injury (the heart attack) it needs time to mend, and this happens in stages. It’s not an overnight fix.
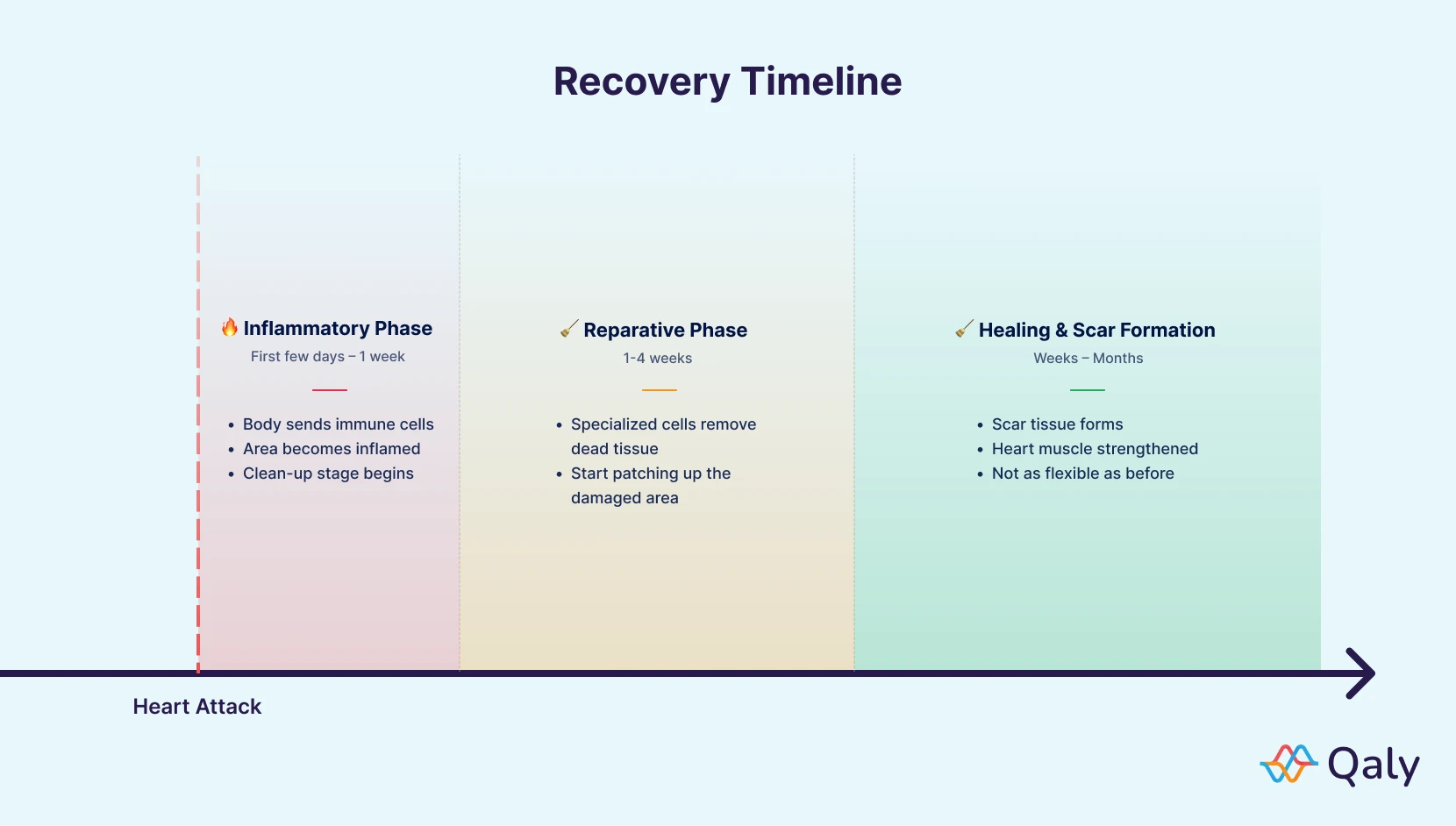
The timeline for this healing process varies a lot from person to person. It depends on the severity of the heart attack, your overall health, and how you were treated. But generally, the damaged area first goes through an inflammatory phase, then a reparative stage where special cells clean things up, and finally, a healing phase where scar tissue forms to strengthen the muscle. This whole process can take anywhere from a few weeks to several months.
A Gentle Guide To Getting Moving Again
The old advice used to be strict bed rest, but we now know that’s not the best path forward. Gentle, gradual movement is crucial for rebuilding your strength and, just as importantly, your confidence. Pushing too hard is a definite risk, but doing nothing at all can actually slow you down.
Here’s a rough idea of what your first month might look like. Remember, this is a guide, not a rulebook. Always listen to your body and stick to the specific plan your medical team gave you.
- Week 1: Your primary job is to rest. Focus on short, slow walks inside your home. Simple things like getting dressed or making a light meal are your "workouts" for now. Avoid lifting anything heavier than 5-10 pounds (think a gallon of milk).
- Week 2: You can start venturing outside for short, easy walks on flat ground. Keep up with light household tasks but steer clear of anything strenuous, like vacuuming or mowing the lawn.
- Weeks 3 & 4: Now you can begin to gradually increase the length and pace of your walks. You might feel up to doing more around the house, like light cooking or folding laundry. This is often when you’ll get the green light to start a formal cardiac rehab program.
To help you track your progress, here’s a simple table outlining some key milestones for your first four weeks.
Recovery Milestones In Your First Month
This table is just a framework. The most important thing is to be patient with yourself and celebrate the small wins along the way.
The Emotional Rollercoaster Is Real
Your physical heart isn't the only thing mending right now - your emotional well-being needs just as much care. It’s incredibly common to feel like you're on an emotional rollercoaster during this first month home.
You might find yourself feeling anxious over every little twinge in your chest. Moments of sadness or even depression can hit as you process what just happened. Some days you might feel irritable or have mood swings that seem to come out of nowhere.
Please hear this: Experiencing these emotions is not a sign of weakness. It's a natural human response to a major, life-threatening event.
Letting yourself feel these things is the first step. Talk to your loved ones; don't bottle it up. If these feelings start to feel too heavy, it's so important to speak with your doctor or a therapist.
The Power of Cardiac Rehabilitation
If there’s one thing you can do to truly take control of your recovery, it’s this: enroll in a cardiac rehabilitation program. This isn't just an exercise class at the local gym. It’s a medically supervised program built specifically for people who’ve had a heart event.
Think of it as your personal comeback team. A typical cardiac rehab program includes:
- Monitored Exercise: You'll safely rebuild your physical strength under the watchful eye of medical pros who know your heart’s limits.
- Education: You get practical advice on heart-healthy eating, managing medications, and lowering your risk factors for the future.
- Counseling and Support: You'll learn stress management techniques and connect with other people who actually get what you're going through.
As you settle back in at home, looking into options like cardiac home health care services can also provide an extra layer of support. This first month is all about setting the stage for a strong recovery. Be patient, be kind to yourself, and lean on your support system. You’ve got this.
Building Strength And New Habits: Months Two To Six
You've made it past the initial shock and the first month of healing. Now, you’re stepping into a new, empowering phase of your heart attack recovery timeline. The next several months are all about shifting gears - moving from careful recovery to actively building a stronger, more resilient future.
Your mindset will naturally pivot from just healing to proactively preventing another heart event. This is where you really start to take the reins. It’s a time for forming new, sustainable habits that will serve you for the rest of your life. We'll walk through how to nourish your body, safely build up your endurance, and handle the emotional side of getting back to a full life.
Embracing A Heart-Nourishing Lifestyle
After a heart attack, the food you eat becomes one of your most powerful tools. But first, let’s get rid of the word "diet." This isn't about restriction or feeling deprived; it’s about discovering a way of eating that truly protects and strengthens your heart.
Think of it as simply upgrading the fuel you put in your body. Instead of dwelling on what you can't have, let's focus on all the great things you can add.
- More Color: Try to fill your plate with a rainbow of fruits and vegetables. They're absolutely packed with heart-protective antioxidants and vitamins.
- Lean Proteins: Make friends with fish (especially those rich in omega-3s like salmon), chicken, beans, and lentils.
- Healthy Fats: Bring in sources like avocados, nuts, seeds, and olive oil to give your cardiovascular system the support it needs.
Safely Building Your Physical Endurance
By now, your cardiac rehab program is likely in full swing, and this is where you'll start to see some incredible progress. The goal is to graduate from short, gentle walks to more sustained, moderate activity that makes your heart muscle stronger without overdoing it.
Your cardiac rehab team is your personal guide on this journey. They'll keep an eye on your heart rate and blood pressure, making sure you're exercising in a way that helps, not harms, your heart. This supervised environment builds not just physical strength but also a tremendous amount of confidence. It's where you learn to trust your body again - a huge mental hurdle to clear.

Remember, consistency is far more important than intensity. A brisk 30-minute walk five days a week is infinitely better for your heart than one grueling, high-intensity workout that leaves you exhausted.
As you get stronger, you can start reintroducing hobbies you love, whether it's getting back in the garden, dancing, or going for a bike ride. To learn more about how to progress safely, check out our guide on exercise after a heart attack for more detailed advice.
Navigating Work, Intimacy, And Hobbies
This period often brings up some very practical and emotional questions about returning to your "normal" life. It's completely common to feel anxious about heading back to work, resuming intimacy, or even just picking up old hobbies. You might find yourself worrying, "Is this safe? What if I overdo it?"
These fears are completely valid. The key here is open communication with your doctor, your partner, and your employer. Easing back into work, maybe with shorter hours at first, can make the transition much smoother. Intimacy, like any physical activity, can be resumed when you feel ready and your doctor has given you the okay. It’s all about listening to your body and pacing yourself.
This is also a time to celebrate how far you've come. Just thinking about these activities is a testament to your progress. Looking forward is a powerful part of the healing process.
Living Your New Normal: Six Months And Beyond
Once you've passed the six-month mark in your recovery, you'll probably notice a real shift. That initial, all-consuming focus on healing begins to settle into a new, more comfortable rhythm. The routines you've worked so hard to establish, those daily walks, mindful meals, and medication schedules, start feeling less like a checklist and more like second nature.
This is your new normal. It's a powerful testament to your resilience and the solid foundation you've built for a long, vibrant life ahead. The game now shifts from short-term recovery to long-term maintenance. This is the phase where you truly learn to thrive, not just survive.
Partnering In Your Ongoing Care
Your relationship with your healthcare team changes, too. Those frequent, intense check-ups of the early months will likely become less common, evolving into more of a long-term partnership. Think of these appointments as your opportunity to be an active, informed driver of your own care.
Before you go to each visit, take a few minutes to reflect on how things have been going.
- How has your energy been?
- Are you noticing any new or returning symptoms?
- How are your medications feeling? Any side effects?
- What's been challenging with your diet or exercise plan?
Coming in with a list of questions and observations turns you into a partner in the process, not just a patient. It gives your doctor a real-world look at your experience, which helps them fine-tune your treatment plan so it keeps working for you.
Long-term monitoring isn't a sign of weakness; it's a smart strategy for lifelong strength. It's like getting a regular tune-up for a classic car you plan to enjoy for many, many years to come.
Staying Motivated For The Long Haul
Let’s be honest, staying motivated is tough. Life gets busy, old habits can be tempting, and the initial urgency of your recovery starts to fade. It's completely normal for that initial burst of enthusiasm to level off, which is why it’s so important to have strategies to keep your healthy habits on track.
One of the biggest hurdles can be managing cholesterol, mainly because its effects aren't something you can see or feel day-to-day. To keep this top of mind, it can be really helpful to dig into the role of cholesterol in heart health to fully grasp why it's so critical for your future.
Here are a few practical ways to keep that fire lit:
- Find Your "Why": Reconnect with your deepest reason for making these changes. Is it to watch your kids or grandkids grow up? To travel the world? To simply feel strong and energetic every single day? Write it down and stick it somewhere you’ll see it often.
- Make It Fun: If you despise the treadmill, don't force it. Find a physical activity you actually love, whether that's hiking, dancing, or swimming. If you're bored with the same healthy meals, grab a new cookbook and start experimenting with exciting, heart-friendly recipes.
- Track Your Wins: Keep a simple journal of your walks, your blood pressure readings, or just how you feel. Looking back and seeing how far you’ve come is an incredibly powerful motivator to keep pushing forward.
Nurturing Your Psychological Well-Being
The recovery journey isn’t just physical. A heart attack is a major life event, and it can leave behind emotional scars. Months later, it's still common to wrestle with anxiety, fear of another event, or waves of sadness.
This is a time for deep self-compassion. Acknowledge these feelings without judging them; they are a perfectly valid part of your story. Your support system of family, friends, and support groups continues to be a lifeline. Don't ever be afraid to lean on them.
This is also a moment to pause, reflect, and celebrate. Look back at where you were six months ago and honor the incredible strength and courage it took to get here. You’ve faced one of life’s biggest challenges and have come out the other side with a new perspective and a renewed resilience. Embrace the future with confidence - you've more than earned it.
Frequently Asked Questions About Recovery
As you navigate the recovery timeline, it's completely normal for questions to bubble up. You've been through a lot, and wondering about the specifics of getting your life back is a natural part of the process. This section is here to tackle some of the most common concerns we hear, offering clear, straightforward answers to give you peace of mind.
When Can I Return To Work After A Heart Attack?
Honestly, there’s no magic number. Your return-to-work timeline is deeply personal and depends on a few key things: the severity of your heart attack, what your job actually entails, and how your own body is healing.
Someone with a desk job might feel ready to ease back in after just two to four weeks. But if your work involves heavy lifting, constant physical exertion, or high-pressure situations, your cardiologist will likely advise waiting closer to two or three months, maybe even longer.
The most critical step is having a frank conversation with your cardiologist and cardiac rehab team. They can help you map out a sensible plan. Often, a gradual return works best, think starting with half-days or working from home for a bit. More than anything, listen to what your body is telling you. Rushing back isn't worth it. Your long-term health is the real prize here.
Is Feeling Depressed Or Anxious Normal During Recovery?
Yes. It's not just normal; it's incredibly common and, unfortunately, not talked about enough. Going through a major, life-threatening event is a huge shock to the system physically and mentally. It’s natural to feel a whole mix of emotions, including depression, anxiety, fear, and even anger, as your mind works to process it all.
These feelings are not a sign of weakness. They are a sign that you are human. The most important thing you can do is talk about it. Open up to your family, a trusted friend, your doctor, or a mental health professional. Cardiac rehab programs are fantastic for this very reason; they often have support groups where you can connect with people who know exactly what you’re going through.
Acknowledging these emotions and seeking support is a profound act of strength. It's a crucial piece of a holistic recovery that honors both your physical and mental well-being.
What Are The Most Important Lifestyle Changes To Make?
Try to think of these as powerful upgrades to your life, not painful sacrifices. While every positive change makes a difference, focusing your energy on a few key areas can have the biggest impact on your heart health and dramatically lower your risk of another event.
These are the four pillars of a heart-healthy lifestyle:
- Heart-Nourishing Eating: This is about shifting your focus to whole, real foods. Think vibrant fruits and vegetables, lean proteins like fish and chicken, and healthy fats from avocados, nuts, and olive oil. The main goal is to cut way back on sodium and heavily processed foods.
- Regular Physical Activity: Consistency is your best friend here. Working with your cardiac rehab team, aim for about 150 minutes of moderate exercise each week. That could be as simple as a brisk 30-minute walk, five days a week.
- Quitting Smoking: If you smoke, this is it. Stopping is the single most powerful thing you can do for your heart. No other change you make will have a greater positive impact.
- Managing Stress: Find healthy ways to navigate life's pressures. This looks different for everyone. It could be mindfulness or meditation, spending quiet time in nature, picking up a hobby you love, or gentle yoga.
How Do I Know If I Am Recovering Well?
Learning to trust your body again can be a real challenge. It's easy to second-guess every little ache or twinge. One of the best signs that you're on the right track is seeing steady, gradual progress. You should be able to do a little more each week without symptoms like chest pain or getting severely out of breath.
Being an active partner in your own care is vital. Never hesitate to bring up your concerns with your doctor. It can be incredibly helpful to jot down a list of questions before your appointments to make sure you cover everything. If you need a good place to start, our article on questions to ask your cardiologist has some great ideas. Remember, this is a team effort, and you are the star player.
At Qaly, we understand that peace of mind is a vital part of your recovery. Our service connects you with certified experts who can interpret your wearable ECGs from devices like Apple Watch, Fitbit, or Kardia in minutes, any time of day. If you’re feeling an unusual flutter or just need reassurance, Qaly provides the expert analysis you need, right from your phone. Learn more about how we can support your heart health journey at Qaly.
Recovering from a heart attack? On the Qaly app, human experts can review your ECGs and help you track your recovery.









.png)
.png)