Key Takeaways
Hello, heart hero. We get it, starting a new medication like verapamil can bring up a lot of questions, especially about side effects. You’ve been prescribed this for a good reason, but it’s completely normal to want to understand what to expect. We're here to walk you through it with clear, supportive information.
Your Guide to Understanding Verapamil
Being an active partner in your health journey is your greatest strength, and that starts with being informed. We know that the healthcare system can sometimes feel impersonal, and it's only natural to feel a bit cautious about a new prescription. Our goal here is to give you clear, reliable information so you can feel confident and in control of your treatment.
This guide will walk you through what it's like to take verapamil in a way that’s easy to understand, without all the confusing medical jargon. We'll cover everything from the most common and manageable issues to the rarer signs that mean it's time to talk to your doctor.
What Is Verapamil and Why Is It Prescribed?
Verapamil is part of a group of medications called calcium channel blockers. Think of calcium as a tiny messenger that tells the muscles in your heart and blood vessels when to squeeze or contract. Verapamil works by gently blocking some of these messages from getting through.
This simple action has a few powerful and helpful effects on your body:
- It relaxes your blood vessels: When the vessels widen, it’s easier for blood to flow through them, which is great for lowering high blood pressure.
- It can slow your heart rate: For certain heart rhythm issues, slowing down the heart's electrical signals can help restore a more stable, normal beat.
- It reduces the heart's workload: By relaxing the blood vessels and sometimes slowing the heart, verapamil takes a lot of strain off your heart muscle.
Because of what it does, doctors often turn to verapamil for conditions like hypertension (high blood pressure), angina (chest pain), and certain arrhythmias (irregular heartbeats).
What Are the Most Common Side Effects?
Like any medication, verapamil can have side effects, but the good news is that most are mild and manageable. The most frequently reported issue, by far, is constipation. Because verapamil is so good at relaxing the smooth muscles in your blood vessels, it can sometimes have the same effect on the muscles in your intestines, slowing things down.
Comprehensive reviews show constipation affects about 7.3% of patients, making it a key side effect to be aware of. While it isn't dangerous, it can definitely impact your quality of life. You can read more about verapamil's effects on Wikipedia.
Other common side effects might include dizziness, headache, or a feeling of fatigue, especially when you first start taking the medication. These often get better as your body gets used to it. We'll explore these and others in more detail throughout this guide, along with practical tips to help you manage them.
How Verapamil Affects Your Heart's Rhythm
Verapamil is designed to help your heart by relaxing your blood vessels and gently slowing down its pace. Think of your heart’s electrical system as a perfectly timed orchestra, with each beat following a steady rhythm. Verapamil helps conduct this orchestra, making sure the music doesn't get too fast or chaotic, which is fantastic for managing conditions like high blood pressure or arrhythmias.
Sometimes, though, this medication can slow the tempo a little more than intended. This is one of the key side effects verapamil can have on your heart's rhythm. For most people, this change is very subtle and doesn't cause any problems. It's just a sign that the medication is doing its job.
The key is to understand what's happening inside your body so you can feel in control. Your doctor might suggest monitoring your heart with an ECG, especially when you first start verapamil. This isn't meant to be alarming; it's a proactive step to ensure the medication is working just right for you, making you an informed partner in your own care.
Bradycardia: Slowing the Beat
One of the most direct effects of verapamil on the heart is its ability to slow your heart rate. When your heart rate drops below 60 beats per minute, it's called bradycardia. Often, a slightly slower heart rate is exactly what we want from the treatment, as it reduces the heart's workload.
Many people with bradycardia caused by verapamil feel perfectly fine and might not even notice it. However, if the heart rate drops too low, it can lead to symptoms like:
- Feeling unusually tired or weak
- Dizziness or lightheadedness
- Shortness of breath
- Feeling faint or actually fainting
These symptoms happen because a very slow heart rate might not be pumping enough oxygen-rich blood to the rest of your body, especially your brain. It's really important to pay attention to how you feel and let your doctor know about any new symptoms.
Understanding Heart Block
Beyond just slowing the heart rate, verapamil can also affect the electrical signals as they travel through your heart. Imagine your heart's electrical pathway is a highway. Verapamil can sometimes create a slight traffic delay at a specific junction called the atrioventricular (AV) node. This delay is known as an AV block.

A first-degree AV block is often a minor change seen on an ECG and usually causes no symptoms. It's like a brief pause at a yield sign. The signal still gets through, just a fraction of a second later.
Higher degrees of AV block are more serious and much rarer, but it’s good to be aware of them. Studies show that the risk of these cardiac events can increase with higher doses. A review of patients taking verapamil for cluster headaches found that 6% developed first-degree AV block and 0.5% experienced second-degree AV block, with the risk being higher for those on more than 720 mg per day. The onset of these issues can sometimes be delayed, appearing months after starting therapy, which highlights why ongoing monitoring is so valuable. You can explore the full study on cardiac adverse events.
Verapamil's effect on your heart's electrical timing is just one of many factors to consider. You can also learn more about other drugs that cause QT prolongation in our detailed guide.
Managing Common Non-Cardiac Side Effects

While verapamil is focused on helping your heart, its effects can sometimes ripple out to other parts of your body. This is completely normal. Understanding these non-cardiac side effects verapamil might cause is the first step toward managing them effectively.
We know new symptoms can be unsettling. But most of these side effects are mild, and you can often manage them with a few simple, practical changes.
The most common side effect, by a long shot, is constipation. Verapamil works by relaxing the smooth muscles in your blood vessel walls, but it also has the same effect on the smooth muscles in your intestines. Think of it like a gentle brake being applied to your digestive system, which can slow things down.
Taming Tummy Troubles
For most people, dealing with constipation is about making small, consistent tweaks to your daily habits. No need to overhaul your entire life to find relief.
Here are a few gentle strategies that can make a big difference:
- Boost Your Fiber: Slowly increase your intake of fiber-rich foods like fruits, vegetables, whole grains, and beans. Fiber adds bulk and helps keep your system moving smoothly.
- Stay Hydrated: Drinking plenty of water is key. It softens everything up, making it easier to pass. Aim for at least eight glasses a day.
- Get Moving: Even a gentle daily walk can stimulate your bowel muscles and help restore regularity.
If these lifestyle changes aren't quite cutting it, don't just put up with it. Talk to your doctor. They might suggest a gentle over-the-counter stool softener or another solution that’s safe to use with verapamil.
Remember, you are your own best advocate. If a side effect is bothering you, it's always worth discussing with your healthcare provider. Your comfort and quality of life are important parts of your treatment plan.
Addressing Swelling and Dizziness
Another non-cardiac effect some people notice is swelling, especially in the ankles and feet. This is called edema. It happens because verapamil widens your blood vessels, which can sometimes cause a tiny amount of fluid to leak into nearby tissues. Gravity often pulls this fluid down to your lower legs.
An easy trick to manage this is to elevate your feet whenever you're resting. This simple action uses gravity in your favor, helping that fluid move back into circulation.
Dizziness, particularly when you stand up too quickly, can also pop up. This happens because the medication lowers your blood pressure, and your body might need an extra second to adjust when you change positions.
The best way to handle this is to simply take your time. When getting out of bed or up from a chair, move slowly. Try sitting on the edge of the bed for a minute before you stand all the way up. This little pause gives your body a chance to adapt and can help prevent that dizzy spell.
For a broader look at how different heart medications can impact you, you can read our guide on the side effects of antiarrhythmic drugs.
Knowing When to Seek Medical Attention

While most of verapamil's side effects are manageable, it’s crucial to know which signs are your body’s way of saying, "Hey, we need to get this checked out." Think of this section as your safety map. It’s here to empower you with knowledge, not to create fear.
Knowing what to look for helps you stay in the driver's seat of your health. It's about learning the difference between a minor detour and a real roadblock on your treatment journey.
Red Flag Symptoms That Need a Doctor's Attention
Sometimes, a side effect is more than just an inconvenience. If you experience any of the following, it's a clear signal to contact your doctor or get medical help right away.
Here are the key warning signs to watch for:
- Severe Dizziness or Fainting: Feeling a little lightheaded when you stand up is one thing. But if you feel like you might pass out, or you actually do, that’s a red flag.
- A Very Slow Heartbeat: If you check your pulse and it seems unusually slow (under 50 beats per minute) and you also feel weak, tired, or breathless, it’s time to call your doctor.
- New or Worsening Chest Pain: Verapamil is often prescribed to treat chest pain (angina). So, any new or worsening chest pain is a serious sign that needs immediate evaluation.
- Sudden or Severe Swelling: A little ankle swelling can be a common side effect, but sudden swelling in your hands, feet, or face, or rapid weight gain, could point to concerning fluid buildup.
- Shortness of Breath: If you suddenly find it hard to breathe, especially when lying down or with minimal activity, this requires urgent attention.
These symptoms are your body’s built-in alert system. Listening to them and acting quickly is a powerful way to protect yourself and ensure your treatment stays on a safe track.
Signs of an Allergic Reaction
Although rare, a severe allergic reaction to any medication is possible. These reactions usually happen fast, often soon after taking a dose, and are considered a medical emergency.
Look out for these signs:
- A Sudden Rash or Hives: An unexpected, itchy, and widespread skin reaction.
- Swelling of the Face, Lips, Tongue, or Throat: This is particularly dangerous as it can make it difficult to breathe or swallow.
- Difficulty Breathing or Wheezing: Any sudden trouble getting air is a critical symptom.
An allergic reaction is a serious matter. If you suspect one, don't wait. Seek emergency medical help immediately.
Understanding Overdose Risk
It's also crucial to take your medication exactly as your doctor prescribed. An accidental overdose of verapamil is a serious medical situation. While rare, severe toxicity can be life-threatening, often showing up as a very slow heart rate, weakness, dizziness, and dangerously low blood pressure. You can discover more insights about verapamil toxicity on DrugBank.
Always stick to the prescribed dose and never take an extra one to "catch up" if you miss one. If you're ever unsure about your medication, it’s always better to be safe and call your doctor or pharmacist. Deepening your knowledge about your heart's health is also key; you can learn more about what is cardiac monitoring in our helpful guide.
Navigating Drug and Food Interactions
Taking any new medication is a bit like introducing a new instrument into an orchestra. For the music to sound right, the new instrument needs to harmonize with all the others. The same is true for verapamil. Its effectiveness and safety really depend on how it gets along with other things you put into your body.
This is why it's so critical to understand potential drug and food interactions. It’s not about memorizing a giant list of do's and don'ts. It's more about being aware of a few key players that can change how verapamil works, so you can have smarter, more productive conversations with your doctor and pharmacist.
The Grapefruit Effect
One of the most famous and surprising interactions with verapamil involves a common breakfast fruit: grapefruit. It might seem odd that a healthy food could cause trouble, but grapefruit and its juice contain compounds that can shut down a key enzyme in your intestines.
This enzyme, called CYP3A4, is responsible for breaking down verapamil before it enters your bloodstream. When it's blocked, way more of the medication gets absorbed than your body is prepared for. This can dramatically spike the concentration of verapamil in your system.
The result is that your normal dose can suddenly act like a much, much higher one. This magnifies the drug's effects and seriously increases the risk of side effects like a dangerously slow heart rate (bradycardia) or a sharp drop in blood pressure.
Because of this potent effect, most doctors and pharmacists will tell you to avoid grapefruit and grapefruit juice completely while you're taking verapamil.
Common Medication Interactions
Verapamil can also interact with a wide range of other medications. Your pharmacist is your best resource for cross-checking your entire medication list, but it helps to be aware of some of the usual suspects.
These include:
- Beta-Blockers: Drugs like metoprolol or atenolol also slow the heart rate and lower blood pressure. Taking them with verapamil can create an additive effect, sometimes slowing the heart down too much or causing heart block.
- Certain Antibiotics and Antifungals: Medications such as clarithromycin or ketoconazole can interfere with the very same enzyme that grapefruit does, leading to higher, potentially toxic levels of verapamil in the blood.
- Statins: Some cholesterol-lowering drugs, particularly simvastatin and atorvastatin, can have their levels increased by verapamil. This raises the risk of muscle-related side effects (like myopathy) from the statin.
- Other Heart Rhythm Medications: Drugs used to manage arrhythmias, like amiodarone or quinidine, can have complex and unpredictable interactions with verapamil that require very close monitoring by your cardiologist.
Always, always make sure your doctor and pharmacist have a complete, up-to-date list of everything you take. This isn't just for prescriptions. It includes over-the-counter medicines, vitamins, and any herbal supplements. Keeping this list current is one of the most important things you can do to prevent harmful interactions and keep the side effects verapamil might cause to a minimum.
Working with Your Doctor for Safe Treatment
Taking verapamil is a collaborative effort, a true partnership between you and your doctor. You're the expert on how you feel day-to-day, and they're the expert on the medicine. When you bring those two perspectives together, you get the best possible plan for your heart health.
It's completely normal to feel a little skeptical about the healthcare system sometimes. That's why being an active, prepared participant in your own care is so powerful. This isn't about second-guessing your doctor's expertise; it's about giving them the clear, high-quality information they need to make the best decisions for you.
To make sure your treatment is both safe and effective, your doctor will likely set up some routine monitoring. This is a standard and reassuring part of the process, designed to catch any potential issues before they become problems.
What to Expect During Monitoring
Monitoring is simply your doctor's way of seeing how your body is responding to verapamil. It helps them fine-tune your dose and ensure you're getting all the benefits with the fewest possible side effects.
Here’s what this usually involves:
- Regular Blood Pressure Checks: Since verapamil is often used to lower blood pressure, your doctor will want to check it regularly, especially when you first start the medication or change your dose. This just ensures it's landing in a healthy range, not too high or too low.
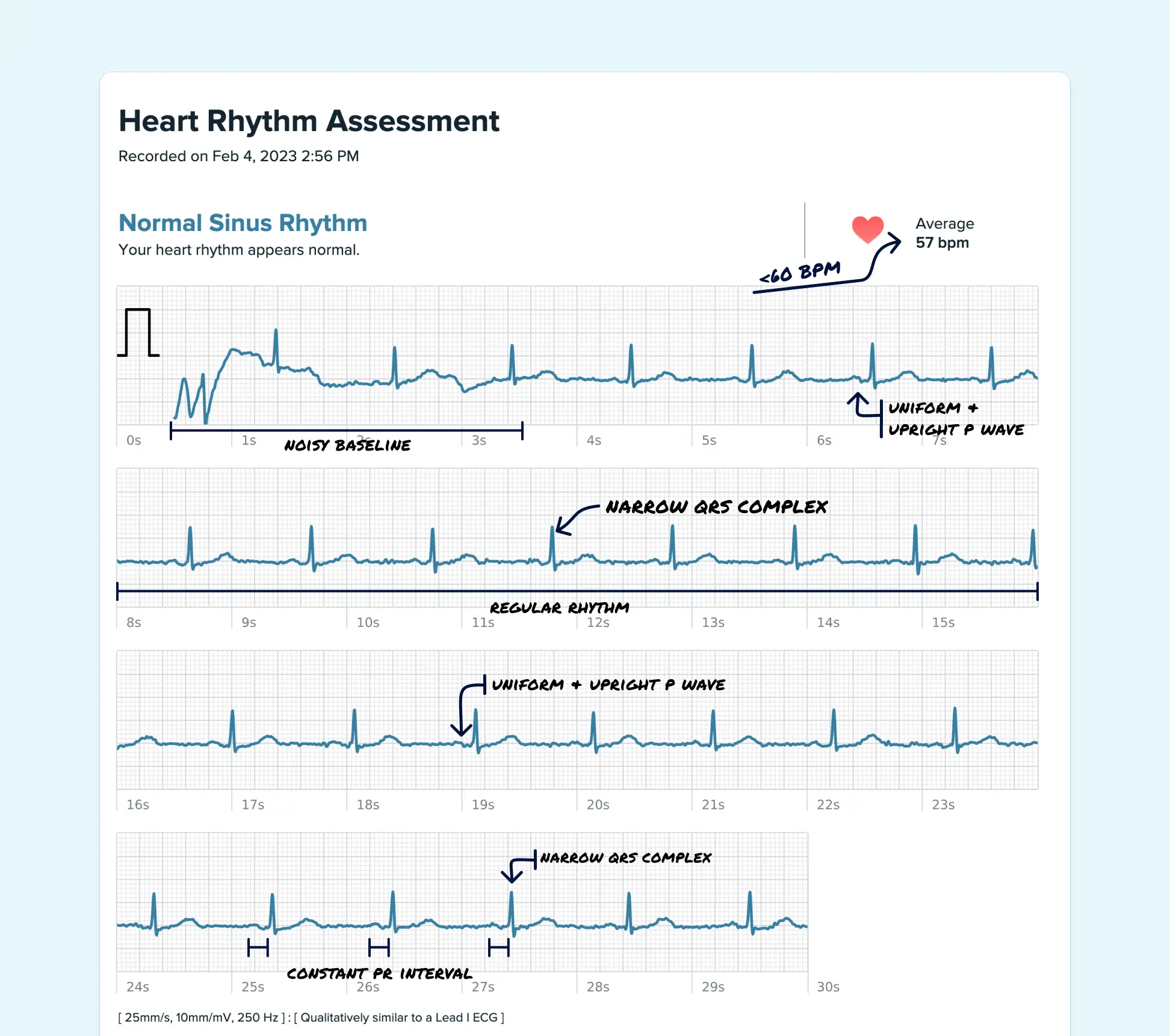
- Occasional ECGs: An electrocardiogram (ECG or EKG) is a quick, painless test that shows your heart's electrical activity. Your doctor might order one to keep an eye on things like a slowed heart rate or a prolonged PR interval, which are known effects of verapamil.
Think of monitoring as a friendly check-in. It's a proactive step that gives both you and your doctor peace of mind, confirming that your treatment plan is perfectly aligned with your body's needs.
Preparing for Your Doctor's Visit
Walking into an appointment prepared can make a world of difference. When you have a plan, you're much more likely to get all your questions answered and leave feeling confident and clear about your treatment.
Here are some key talking points and questions to bring with you:
- Describe Your Symptoms with Detail: Instead of just saying, "I feel dizzy," try being more specific. For example: "I've noticed I get lightheaded for a few seconds almost every time I stand up from my chair." Keeping a simple symptom log on your phone or in a notebook can be a huge help.
- Ask About Your Dosage: If side effects are bothering you, don't hesitate to ask, "Is this the right dose for me, or is there any room to adjust it?" Sometimes a very small tweak is all it takes.
- Discuss Any Side Effects Openly: Be honest about anything you're experiencing, no matter how minor it seems. You could ask, "I've been dealing with more constipation since starting this medication. Are there any safe ways I can manage this?"
- Talk About Monitoring: Show you're engaged in your care. You can ask, "How often should I be checking my blood pressure at home?" or "When would you recommend my next ECG to check on my heart rhythm?" This signals that you're a proactive partner in managing the potential side effects verapamil can cause.
Frequently Asked Questions About Verapamil
We know that starting a new medication brings up a lot of questions. It's completely normal to wonder about these things, and looking for answers means you're taking a thoughtful, active role in your own health.
Let's walk through some of the most common questions people have when they start taking verapamil.
How Long Do Verapamil Side Effects Last?
This is a great question, and the answer really depends on the specific side effect. Many of the initial feelings, like a headache or a bit of dizziness, are often temporary. They usually get better within a few days to a few weeks as your body adjusts to the new medication.
On the other hand, some effects like constipation can be more persistent and might stick around as long as you're taking verapamil. If any side effect is really bothering you or just won't go away, it's always best to have a chat with your doctor. They can often suggest simple fixes or make adjustments to help you feel better.
Can I Stop Taking Verapamil If I Have Side Effects?
This is incredibly important: you should never stop taking verapamil suddenly without talking to your doctor first. Hitting the brakes on this medication can cause a rebound effect, potentially leading to a sharp spike in your blood pressure or making the very heart condition it's supposed to treat even worse.
Think of it this way: if the side effects are tough to handle, see it as a signal to team up with your doctor, not to stop treatment on your own. Your safety comes first, and they are your partner in finding a solution. That might mean adjusting the dose or even trying a different medication altogether.
Does Verapamil Cause Weight Gain?
Verapamil isn't known to cause weight gain from fat directly. However, some people do experience fluid retention, which can show up as swelling (edema) in the ankles and feet. Naturally, this extra fluid can make the number on the scale tick up a bit.
If you notice any sudden or significant weight gain, it's really important to let your doctor know. It could be a sign of fluid buildup that needs attention to keep you safe and comfortable.
Is It Safe to Drink Alcohol While Taking Verapamil?
It’s smart to be very cautious with alcohol when you're on verapamil. Alcohol can amplify the medication’s blood-pressure-lowering effects. This combo can dial up your risk of dizziness, lightheadedness, and even fainting, which could easily lead to a fall and an injury.
For your own safety, the best bet is to limit or avoid alcohol. Be sure to discuss your habits with your doctor so they can give you personalized advice based on your whole health picture. Your proactive questions help make sure every part of your lifestyle is supporting your heart health journey.
Qaly connects you with certified experts who can interpret your readings in minutes. Get clarity on your heart rhythm and peace of mind on your treatment journey










.png)
.png)