Key Takeaways
Yes, beta-blockers are a common and effective first-line treatment for managing Premature Ventricular Complexes (PVCs), especially when they cause bothersome symptoms. They work by calming the heart's electrical system, reducing both the frequency of these extra beats and the anxiety that often comes with them.
What Are PVCs and Why Do They Happen?
Hello heart hero. If you’ve ever felt a strange flutter, a skipped beat, or a sudden thump in your chest, you’ve likely experienced a Premature Ventricular Complex, or PVC. It’s a sensation that can feel alarming, and it’s natural to feel worried. Taking the time to understand what’s happening inside your body is a powerful first step toward feeling back in control.

A Little Hiccup in Your Heart's Rhythm
Think of your heart as a perfectly synchronized orchestra, with a main conductor, your sinus node, keeping a steady beat. A PVC is like a musician in the lower chambers (the ventricles) getting a little too eager and playing a beat just before it’s their turn.
This early beat is often weaker than a normal one. It’s followed by a brief pause as your heart's electrical system resets itself. Then, the next beat comes through with extra force to push out the blood that accumulated during the pause. That powerful beat is the "thump" you feel, and the pause is the "skipped beat" sensation.
You Are Far from Alone
One of the most important things to know is just how incredibly common PVCs are. The truth is, nearly everyone has them from time to time, even people with perfectly healthy hearts. It can be a huge relief to learn that what feels so strange is actually a very shared human experience.
The incidence of PVCs is remarkably high, estimated to be between 4% and 50% in the general population. Data from one study even found that 99.5% of elderly participants had at least one PVC when monitored with continuous patch devices. Read more about the prevalence of PVCs in this study.
What Triggers These Extra Beats?
Often, PVCs don’t have a clear cause, but certain triggers can make them more frequent or noticeable. Recognizing these can be an empowering first step in managing them on your own terms.
Common triggers include stress and anxiety, caffeine and alcohol, lack of sleep, and electrolyte imbalances. When you're stressed, your body releases hormones like adrenaline, which can make heart cells more excitable. Caffeine and alcohol can directly affect the heart's electrical signaling in some individuals. Fatigue puts a strain on your entire body, including your heart's finely tuned rhythm. And levels of minerals like potassium and magnesium are crucial for proper heart function.
When to Pay Closer Attention
The vast majority of occasional PVCs are completely harmless. However, if they become very frequent or cause significant symptoms like dizziness, lightheadedness, or constant anxiety, it’s a good idea to chat with a healthcare provider you trust.
The goal isn't always to eliminate every single extra beat, but to reduce the symptoms and ensure there isn't an underlying issue causing them. For a deeper dive, you can learn more about premature ventricular contractions (PVCs) in our detailed guide. Understanding your own patterns is the foundation for a productive conversation about your health.
How Beta-Blockers Gently Calm the Heart
We've talked about what those frustrating PVCs are, and now it's time to dive into one of the most common ways to help calm them down. If a doctor has mentioned using beta-blockers for PVCs, you might be wondering what they actually do inside your body. It can feel unsettling to take a medication without truly understanding how it works, so let's gently pull back the curtain.
Think of adrenaline as your body's natural hype music. It cranks up the volume on your heart, making it beat faster and more forcefully. When you're stressed, anxious, or even just had too much caffeine, your body releases these stress hormones. This "loud music" can make your heart's electrical system a little jumpy, making it more likely to fire off those premature, extra beats we call PVCs.
This is where beta-blockers come in. They act like a volume knob for that hype music. They don't turn it off completely, but they gently turn it down to a much more manageable level. By doing this, they help your heart beat slower and with less force, creating a calmer, more stable environment where those extra beats are less likely to occur.
The Science Behind the Calm
So, how do beta-blockers achieve this calming effect? They work by blocking specific sites in your heart called beta receptors. You can think of these receptors as docking stations for stress hormones like adrenaline.
When adrenaline docks with these receptors, it tells your heart to ramp things up. Beta-blockers fit neatly into these docking stations, essentially blocking adrenaline from delivering its high-energy message. This is why they are often the first choice for symptomatic PVCs. They directly counter one of the most common triggers, the body's own stress response.
This targeted action is what makes beta-blockers so effective. They don't just mask symptoms; they address a root cause of excitability in the heart's electrical system, helping to restore a more peaceful and regular rhythm.
This mechanism is also why you might feel a general sense of calm while taking them, as they can dampen the physical symptoms of anxiety, like a racing pulse. It’s a dual benefit that many people find incredibly reassuring.
Common Beta-Blockers for PVCs
While there are many types of beta-blockers, a few are more commonly used to help manage PVCs. Your doctor will choose one based on your specific health profile, but some of the names you might hear include Metoprolol, Atenolol, and Propranolol.
Metoprolol is a "cardioselective" beta-blocker, meaning it primarily targets the beta receptors in your heart. This focus can sometimes lead to fewer side effects elsewhere in the body. Atenolol is similar to Metoprolol and is another cardioselective option frequently prescribed. Propranolol is a "non-selective" beta-blocker, which means it blocks beta receptors in other parts of the body, not just the heart. This can be useful for people who also experience physical symptoms of anxiety, like tremors.
It's important to remember that finding the right medication and the right dose is a partnership between you and your doctor. What works wonderfully for one person may not be the best fit for another, and that's perfectly okay.
The journey often starts with a low dose, which is then gradually adjusted to find that sweet spot where your symptoms improve with minimal side effects. Understanding how these medications work with your heart can be empowering. You can learn more about how beta-blockers affect your heart and ECG in our detailed article. Ultimately, the goal is to help your heart's orchestra find its steady, comfortable rhythm once again.
The Real-World Effectiveness of Beta-Blockers for PVCs
When you're dealing with the unnerving sensation of PVCs, the biggest question on your mind is simple: will this treatment actually work? It’s a totally fair question. After all, nobody wants a one-size-fits-all answer for something so personal. So, let's have an honest conversation about how effective beta-blockers really are for PVCs, because the answer isn't always as simple as we'd like.
The truth is, how well beta-blockers work is different for everyone. For some people, they’re a game-changer, dramatically calming down those startling thumps and flutters. For others, the improvement might feel more subtle. The key thing to understand is that "success" with this treatment isn't always about eliminating every single extra beat.
Moving Beyond Just Feeling Better
While feeling better is a huge part of the goal, your cardiologist is also looking at a key metric called PVC burden. Think of it as the percentage of your total heartbeats that are PVCs. For example, a 5% burden means that five out of every 100 beats are premature. A primary goal of beta-blockers is to bring this number down.
Even if the medication only drops your burden from, say, 15% down to 8%, that’s a significant victory for your heart's long-term health. The aim isn't just about feeling fewer flutters today; it's about creating a healthier, more stable environment for your heart for years to come. This is where the true, and often unseen, power of beta-blockers really shines.
The most important takeaway is that beta-blockers do more than just quiet down symptoms. By reducing the overall strain and excitability of the heart, they offer protective benefits that contribute to your long-term cardiovascular well-being, even if some PVCs remain.
The Bigger Picture: Your Heart's Long-Term Health
This long-term protection is a critical point that often gets lost when we only focus on immediate symptom relief. While beta-blockers might only moderately reduce the number of PVCs you feel, their real value is in safeguarding your heart over time. Research consistently shows that managing arrhythmias with treatments like beta-blockers is tied to better long-term outcomes.
One comprehensive analysis looked at patient outcomes over a 10-year period. It found that patients with a high burden of premature beats who were treated with beta-blockers had an incredible 48% risk reduction in long-term all-cause mortality compared to those who weren't treated. The study also showed up to a 40% risk reduction in mortality for the overall treatment group, highlighting the profound protective effects of this therapy. You can explore more about these long-term mortality benefits in the published research.
This is exactly why doctors often recommend them even if they don't erase every symptom. The therapy is playing defense for your heart, reducing risks you can't see or feel day-to-day. It’s a proactive strategy for a healthier future.
What Does Success Look Like for You?
Because everyone’s experience with PVCs is unique, success with beta-blockers is deeply personal. It's not a simple pass-or-fail test. Instead, "working" can mean a few different things, and it’s important to recognize what a win looks like for you.
Success might mean a noticeable reduction in symptoms so you feel fewer thumps and flutters. It could also mean less anxiety; just feeling the medication calm your heart's forceful beats can break the cycle of worry that PVCs often trigger. Peace of mind is a powerful measure of success. Finally, it could be a medically significant drop in PVC burden. Even if you still feel some PVCs, your doctor may see a meaningful reduction in your PVC frequency on an ECG, confirming the medication is protecting your heart.
Ultimately, the goal is a partnership between you and your doctor to find the best path forward. Beta-blockers are a valuable tool, not a magic wand to make PVCs disappear forever, but a steadying hand to calm your heart, ease your mind, and protect your health for the long run.
Determining If Beta-Blockers Are Right for You
Deciding on a treatment path for PVCs can feel overwhelming, especially when a one-size-fits-all solution just doesn't feel right. The good news is that the best approach is always a personalized one. Your unique heart patterns and symptoms are the most important clues in figuring out if beta-blockers are the right first step for you.
There's no magic formula here. Instead, your doctor will look for specific signs that suggest you might respond particularly well to beta-blockers. It’s all about moving away from a trial-and-error approach and toward a decision guided by your body's own data.
Clues That Point Toward Beta-Blockers
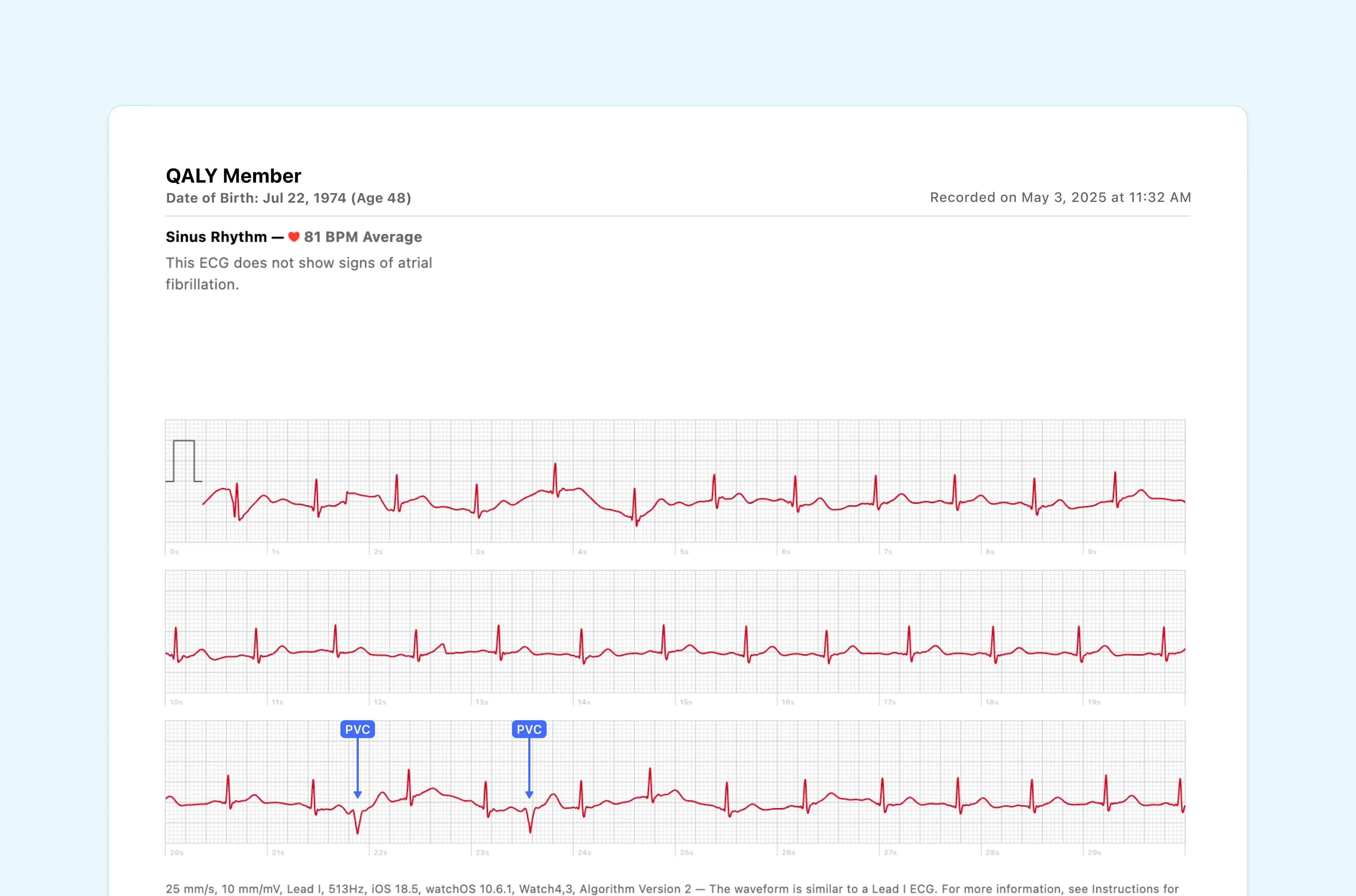
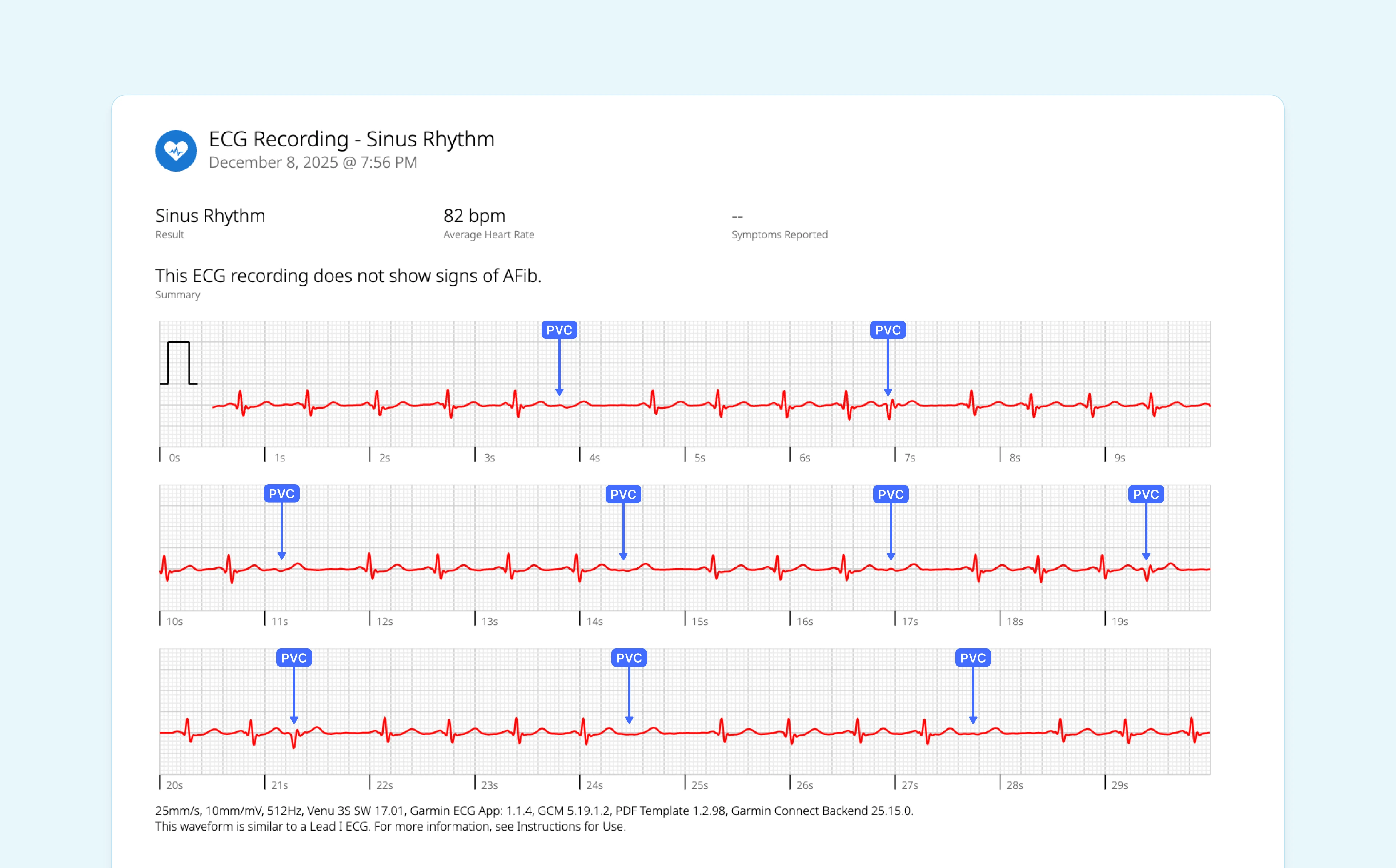
Think of your heart's data, like the readings from a wearable ECG, as a personal roadmap. Certain details on this map can guide your clinician toward beta-blockers as a strong starting point.
One of the biggest indicators is a clear connection between your PVCs and your heart rate. If your PVCs tend to pop up more often when your heart is beating faster, like during exercise or times of stress, it’s a strong sign that adrenaline is a key trigger. Since beta-blockers work by turning down adrenaline's "volume," they are often very effective in these situations.
The key takeaway here is that the treatment journey is a process of evaluation. The first goal is improving your quality of life, followed by sustaining your cardiovascular health for the long run.
Using Your ECG Data to Predict Success
Modern research is uncovering even more specific ECG markers that can predict who will benefit most from beta-blockers versus other medications like calcium channel blockers. This is where detailed monitoring becomes so valuable.
A recent study found that while the response to treatment was nearly split between beta-blockers (45.5%) and calcium channel blockers (54.5%), distinct ECG patterns emerged for each group. Patients who did well on beta-blockers often had a higher average heart rate and specific characteristics on their ECG, like a longer PVC QRS duration. These subtle details, captured by precise monitoring, can help predict treatment success before you even start. You can learn more about the electrocardiographic markers that predict treatment response in the full study.
This is empowering. It means your treatment can be guided by solid evidence from your own heart, not just guesswork.
The goal is to match the right medication to your specific type of PVC. Detailed data helps your doctor understand the 'personality' of your extra beats, leading to a more targeted and effective treatment plan from the start.
When Other Treatments Might Be Better
On the flip side, if your PVCs are more common when your heart rate is slow, or if they have certain other ECG characteristics, your doctor might consider a different class of medication, like calcium channel blockers, as a better first choice.
This highlights why continuous monitoring with a wearable device is so helpful. The more information you and your clinician have about when and how your PVCs occur, the clearer the path forward becomes. You become an active partner in your care, providing the very data that helps tailor your treatment.
Navigating Side Effects and Treatment Alternatives
Starting a new medication is a big step, and it's completely normal to have questions about what to expect. While beta-blockers are a trusted option for calming PVCs, it's also true they can bring some side effects. Let's talk about them honestly, not as scary deal-breakers, but as manageable issues you can work through with your doctor.
The goal is always to find a balance where the benefits far outweigh any downsides. Many people who try beta-blockers for PVCs find that any initial side effects are mild and simply fade as their body adjusts.
Understanding Common Beta-Blocker Side Effects
Because beta-blockers work by gently turning down the volume on adrenaline, some of the most common side effects are directly related to this calming effect. They're often dose-dependent, which means a lower dose might not cause them at all.
You might experience fatigue or tiredness, dizziness or lightheadedness, cold hands and feet, or difficulty sleeping or vivid dreams. Feeling a bit more wiped out than usual is the most common side effect, especially when you first start. Dizziness can happen as the medication slows your heart rate and lowers blood pressure. Reduced circulation to your extremities can sometimes make your fingers and toes feel chilly. And while less common, some people notice changes in their sleep patterns.
It's important to see these not as stop signs, but as conversation starters with your doctor. Often, a simple tweak to the dose is all it takes to find that sweet spot for your body.
Empowering Alternatives When Beta-Blockers Aren't the Right Fit
Your journey to a calmer heart is uniquely yours, and beta-blockers are just one possible path. If you're hesitant about medication or if they just don't agree with you, you have other powerful options. Feeling in control of your health means knowing all the roads available to you.
Lifestyle Changes: The Foundation of Heart Rhythm Health
Never underestimate the impact of simple, daily habits. For many people, these adjustments can dramatically reduce PVCs without any medication at all.
Stress management is a great place to start. Since stress is a major PVC trigger, finding ways to unwind is crucial. Techniques like mindfulness, deep breathing exercises, or even just a quiet walk can soothe your nervous system and, in turn, your heart. Balancing electrolytes is also key. Minerals like magnesium and potassium are essential for your heart's electrical stability. You can boost your intake through foods like almonds, spinach, and cashews, or discuss supplementation with your doctor. Finally, prioritizing sleep is vital. A well-rested body is better equipped to maintain a steady heart rhythm.
Other Medical Options Beyond Beta-Blockers
If lifestyle changes aren't quite enough but beta-blockers aren't a good match, your doctor has other tools to consider. This ensures your treatment is tailored specifically to you.
Remember, the goal isn't to force one type of treatment to work. It's about finding the specific strategy that best fits your body, your lifestyle, and your comfort level, putting you in the driver's seat of your own health journey.
Two common medical alternatives include calcium channel blockers and catheter ablation. Calcium channel blockers are another class of medication that can be very effective for PVCs. They work a bit differently than beta-blockers by relaxing blood vessels and slowing the heart rate through a different mechanism. If you want to learn more, check out our guide on understanding calcium channel blockers and how they work. For those with a very high PVC burden or severe symptoms that don't respond to medication, catheter ablation is a highly effective option. It’s a minimally invasive procedure where a specialist carefully maps the heart's electrical system to find the exact spot causing the PVCs and neutralizes it.
How to Monitor Your PVCs with a Wearable ECG
Feeling those heart flutters can be unnerving. It’s natural to want more control and a better understanding of what’s going on. The good news is you don't have to just wait for your next doctor's appointment. Modern technology, like the ECG feature on your smartwatch, puts a powerful tool right on your wrist, turning you into an active partner in managing your heart health.
This isn’t about trying to be your own cardiologist. It's about gathering good, solid information so you can have a much more productive conversation with your doctor. You can go from saying, "I feel like my heart flutters sometimes," to showing them, "I recorded five PVCs in one minute after my morning coffee yesterday." See the difference?
Turning Raw Data into Real Insights
A wearable ECG does more than just show you a squiggly line. It helps you connect the dots between your daily life and your heart rhythm. By taking readings at key moments, you can start to spot patterns that were once completely invisible.
Think of it as keeping a detailed journal of your heart's activity. You can start answering the critical questions that guide your treatment, especially if you're taking beta-blockers for PVCs. You can spot your triggers: do PVCs pop up after a stressful meeting or a poor night's sleep? You can connect symptoms to data by taking an ECG the next time you feel a flutter. And you can monitor your treatment by tracking how often you have PVCs to see if the medication is working.
For those looking into different wearable devices, some general information on new or pre-owned Apple Watches might be useful, as they are one of the popular options with these capabilities.
Making Your Data Count in the Clinic
Here’s the thing: just having a bunch of ECG strips isn't that helpful on its own. The real magic happens when you turn that raw data into something your doctor can easily use. This is where services that analyze at-home ECGs come into play.
These services bridge the gap between just collecting data and actually using it. They can give you an accurate PVC count and create a professional, easy-to-read report from your home recordings, making your personal health data clinically relevant.
Instead of handing your doctor a stack of random readings, you can present a clear summary of your heart's activity over time. This turns your personal observations into a powerful dataset that helps your doctor make better decisions for you. It also gives you the confidence that your concerns are backed by solid evidence. You can learn more about how a portable electrocardiogram monitor can empower your health journey in our detailed guide.
This proactive approach puts you firmly in the driver's seat of your own health. It helps ensure that your treatment plan, whether it involves beta-blockers, lifestyle changes, or something else, is truly tailored to your unique heart and your life.
Common Questions About Beta-Blockers and PVCs
It’s totally normal to have a lot of questions when you're thinking about treatment for PVCs. You might even be a little skeptical about starting a new medication, and you deserve clear answers. Let's walk through some of the most common concerns people have.
How Long Until Beta-Blockers Start Working for PVCs?
You might feel some of the effects pretty quickly, like a calmer, slower heart rate, sometimes within a few hours of your first dose. But seeing the full benefit for actually reducing your PVCs can take several weeks of consistent use.
Think of it like your heart is being gradually retuned. Your doctor will almost always start you on a low dose and then slowly adjust it over time, watching how your symptoms and ECG readings respond. Patience is really important during this initial phase.
Can I Stop Taking Beta-Blockers If My PVCs Go Away?
This is a big one: do not stop taking beta-blockers suddenly without talking to your doctor first. Quitting cold turkey can trigger a rebound effect, which could mean a sudden spike in your heart rate or blood pressure. It can feel pretty unpleasant and be risky.
If you and your doctor agree it's time to stop, they'll create a plan to taper you off the medication slowly and safely. And remember, even if your PVCs have disappeared, the medication might be providing other important protective benefits for your heart that you can't feel.
Will I Have to Take Beta-Blockers for Life?
Not always. How long you'll need them really depends on your unique health situation. For some people, PVCs are kicked off by something temporary, like a period of intense stress or a viral illness. In those cases, medication might only be needed for a short time.
For others who have an underlying heart condition or just very stubborn symptoms, beta-blockers might be a long-term solution. The goal is always the same: use the lowest effective dose for the shortest time necessary to keep you feeling good and your heart healthy.
This is where regular check-ins with your doctor are crucial. When you can bring them clear data from your wearable ECG, you can work together to figure out the best long-term plan for you.
Navigating your heart health journey is easier when you have clear, trustworthy data. With Qaly, you can get your wearable ECGs analyzed by certified experts in minutes.










.png)
.png)