Key Takeaways
Hello Heart Hero. If you've just been told you need blood thinners for AFib, it's completely normal to feel a little overwhelmed. Hearing that phrase can bring up a mix of confusion and genuine concern. If that's you, you're not alone. The healthcare system can sometimes make you feel like just another number, but taking the time to truly understand your treatment is the first step toward regaining control.
Think of this guide as your calm, clear starting point. It's here to answer your questions and, hopefully, replace that uncertainty with confidence.

We'll start by exploring exactly why managing AFib is so critical for your long-term health, with the main goal being one thing: preventing a stroke. You’re not just managing a condition; you're actively protecting your future.
Understanding the AFib and Stroke Connection
So, how does an irregular heartbeat lead to a higher risk of stroke? The connection is more straightforward than it sounds.
Imagine your heart's upper chambers, the atria, as a smoothly flowing river when your heart is beating normally. But with AFib, that smooth river turns into a slow, swirling pool. When blood doesn't move efficiently, it can stagnate.
This pooling creates the perfect storm for blood clots to form. If a small piece of one of these clots breaks off, it can travel through your bloodstream straight to the brain, where it can block a vessel and cut off blood flow. That’s what causes an AFib-related stroke, and it's the primary risk doctors want to prevent.
It’s important to know that AFib is a very common condition. In 2021, an estimated 52.5 million people worldwide were living with it, and that number keeps climbing. This means millions of others are navigating the very same questions you are.
What Does a 'Blood Thinner' Really Do?
Let's clear up one of the most common points of confusion: the name "blood thinner." It's a bit of a misnomer. These medications, more accurately called anticoagulants, don't actually change the thickness or consistency of your blood at all.
Instead, they work by interrupting the complex chemical chain reaction that allows a blood clot to form in the first place. By making it much harder for these dangerous clots to develop inside the heart, they significantly lower the chance of an AFib-related stroke. It's a protective measure, not a cure for the AFib itself.
Your prescription isn't just a pill; it's a shield. It's a proactive strategy to safeguard your brain and body from the most serious complication of atrial fibrillation.
Our goal here is to empower you. By learning about your condition and the treatments available, you become an active, informed partner in your own healthcare. Knowledge is the best tool for turning anxiety into action and taking charge of your heart health journey.
Why Blood Thinners Are Key for AFib Stroke Prevention
If your doctor has brought up the topic of blood thinners, you're probably wondering exactly why they're so important. Let's clear up the confusion. This isn't just a routine prescription; it's a very specific strategy with one critical goal: lowering your risk of having a stroke.
When your heart slips into AFib, the upper chambers don't contract in a strong, coordinated rhythm. Instead, they quiver. This chaotic movement lets blood get sluggish and pool up, which unfortunately creates the perfect environment for clots to form. If one of those tiny clots breaks free and travels to the brain, it can block a vital blood vessel and cause a devastating stroke.
Imagine a smoothly flowing river. Now, picture a small whirlpool forming at the river's edge, trapping leaves and debris and spinning them around. AFib creates a similar effect inside your heart, making it much easier for blood cells to clump together into a clot. This is the exact problem that blood thinners for AFib are designed to prevent.
Your Personal Stroke Risk Matters
It's completely normal to be wary of a one-size-fits-all medical plan, and the good news is, this isn't one. Your doctor doesn't recommend blood thinners to everyone with AFib. Instead, they use a specific tool to personalize this decision for you.
That tool is a scoring system called the CHA₂DS₂-VASc score. The name sounds a bit technical, but the concept behind it is straightforward. It’s essentially a checklist that helps your doctor add up points based on specific risk factors you might have.
These risk factors include things like:
- Your age (stroke risk goes up as we get older)
- Whether you have high blood pressure
- A history of diabetes
- Previous strokes or blood clots
- Any issues with heart failure
Each of these factors adds a point or two to your total score. The higher your score, the higher your personal risk of an AFib-related stroke, which makes the protective benefit of a blood thinner that much more important for you. This calculation ensures the recommendation is based on your unique health profile. For a closer look at how these factors shape treatment decisions, check out our guide on atrial fibrillation anticoagulation guidelines.
A Proven and Essential Treatment
Blood thinners are a well-established method for reducing stroke risk in individuals with all types of atrial fibrillation. This approach is supported by decades of strong evidence demonstrating their effectiveness. Their important role is evident in the demand for AFib medications.
The decision to start a blood thinner is a proactive partnership between you and your doctor. It's about looking at your specific risk factors and using a proven tool to protect your brain and your future health.
Understanding that this is a personalized medical choice, not a blanket rule, can help you feel more confident and in control. It's all about weighing the immense benefit of preventing a stroke against the manageable risks of the medication, a topic we'll explore in more detail later. Taking this protective step is a cornerstone of modern AFib management.
Types of Blood Thinners for AFib: Finding the Right Fit for You
When you're told you need a blood thinner, it's easy to assume it's just one type of pill. But knowing you have choices is empowering, especially when a one-size-fits-all approach doesn't feel right for you. Let's walk through the two main types of blood thinners for Afib: the long-standing medication, warfarin, and the newer group called DOACs.
Think of it like choosing a car. You could go with a classic, reliable model that’s been on the road for decades, or you could opt for a modern vehicle packed with the latest technology. Both can get you where you need to go safely, but they operate very differently and require different kinds of maintenance.
This infographic shows the simple but critical reason these medications are so necessary: Afib lets blood pool in the heart, which can lead to clots that travel to the brain and cause a stroke.
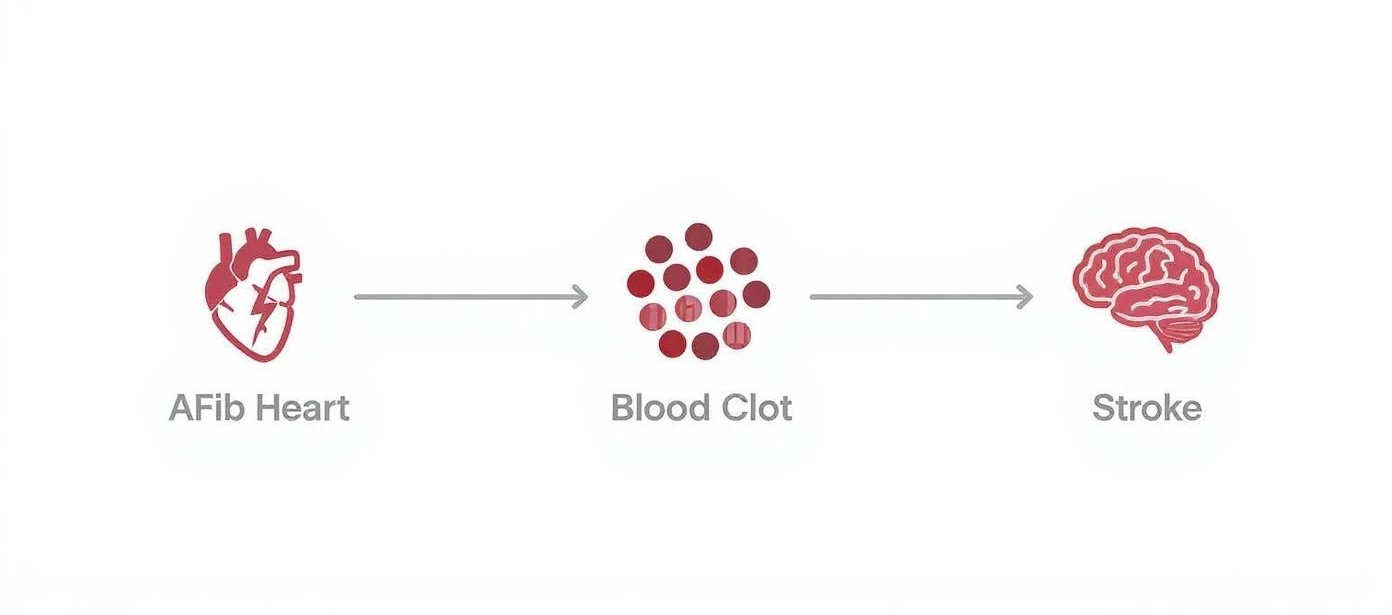
This clear visual shows exactly why interrupting that clot-forming process is the central goal of anticoagulation in Afib.
The Classic Choice: Warfarin
Warfarin is the traditional blood thinner that has been used successfully for over 60 years. It’s a well-understood medication that works by reducing the effects of Vitamin K, a key ingredient your body uses to form blood clots. Because it's been around for so long, doctors have a great deal of experience with it.

However, using warfarin requires a bit more hands-on management.
- Regular Blood Tests: You'll need frequent blood tests, especially at first, to check your INR (International Normalized Ratio). This test measures how long it takes your blood to clot and ensures your dose is in the correct therapeutic range, not too high and not too low.
- Consistent Vitamin K Intake: Since warfarin interacts with Vitamin K, you don't have to avoid foods rich in it (like spinach and kale). The key is keeping your intake consistent from day to day. A sudden salad binge or cutting out greens entirely can throw your INR levels off.
- Dose Adjustments: Your doctor will adjust your dose based on your INR results, lifestyle, and other medications you might be taking.
Think of managing warfarin like balancing a seesaw. The goal is to keep your INR level just right. Those regular check-ins are crucial for maintaining that perfect balance and keeping you safe.
The Modern Option: DOACs
In the last decade or so, a newer class of medications called Direct Oral Anticoagulants (DOACs) has become a common first choice. You might recognize them by their brand names, like Eliquis (apixaban) or Xarelto (rivaroxaban). They work differently than warfarin by directly blocking specific clotting factors in your blood.

DOACs offer a much more streamlined experience for many people.
- Fixed Dosing: They are typically taken as a fixed dose once or twice a day, without the need for constant adjustments.
- No Routine Blood Monitoring: One of the biggest advantages is that you don't need regular INR blood tests. This is a game-changer for many patients.
- Fewer Interactions: They have far fewer interactions with foods, meaning you don't have to worry about your Vitamin K intake.
This convenience and predictability have made DOACs incredibly popular. In fact, the market for Afib medications, valued at around $24.6 billion, is projected to more than double by 2033, largely driven by the adoption of effective anticoagulants like these.
How Your Doctor Helps You Choose
So, which one is right for you? This decision is a perfect example of shared decision-making between you and your doctor. They’ll look at your whole health picture. For instance, they might recommend warfarin if you have certain types of mechanical heart valves or specific kidney issues.
On the other hand, a DOAC might be suggested for its convenience and lower risk of certain types of bleeding, especially bleeding in the brain. Of course, cost and insurance coverage also play a role, as DOACs can be more expensive. This is just one piece of your overall treatment plan; you can learn more about other heart medicine for AFib in our comprehensive guide.
Ultimately, both warfarin and DOACs are highly effective at preventing strokes caused by Afib. The best choice is the one that fits your health profile, lifestyle, and preferences, ensuring you can take it consistently and safely.
Living Well and Safely with Blood Thinners
Starting any new medication can feel like a big deal, and it's completely normal to wonder how it will fit into your daily life. For many people starting blood thinners, there's a nagging unease, especially about the risk of bleeding. This section is all about giving you practical, real-world advice and reassurance. Living a full life on a blood thinner isn't just possible, it's the goal.
The idea isn't to wrap yourself in bubble wrap. It's simply about living with a bit more awareness. With a few small adjustments, you can continue to lead an active, confident life while giving yourself the best protection against an AFib-related stroke.
Understanding and Managing Bleeding Risk
The most common question I hear is, "What if I get a cut?" It’s a perfectly valid concern. After all, the medication works by making it harder for your blood to clot, which means minor cuts or bruises are going to be more noticeable than they were before.
A small nick from shaving might bleed for a little longer. You might also see bruises pop up more easily if you bump into the corner of a table. These things are typically not a cause for alarm; in fact, they're signs the medication is doing its job.
The key is learning to tell the difference between a minor nuisance and something that needs a doctor's attention.
Think of it this way: a blood thinner doesn't make you fragile, it just asks you to be a little more mindful. Knowing what to watch for is the first step toward feeling confident and in control of your health.
Here are a few simple, everyday precautions you can take to minimize any risks:
- Use a soft-bristled toothbrush and be gentle when you floss to protect your gums.
- Opt for an electric razor over a blade razor to reduce the chance of nicks and cuts.
- Take a little extra care when using sharp knives in the kitchen or tools for your hobbies.
- Wear gloves when you're gardening or doing yard work to prevent scrapes.
Creating a Consistent Medication Routine
When it comes to blood thinners, consistency is your best friend. Sticking to a regular schedule helps ensure the medication is working effectively around the clock. If you happen to forget a dose, your doctor or pharmacist can give you specific advice on what to do, never just double up on your next dose.
It's also crucial to keep all of your healthcare providers in the loop. Always tell every doctor, dentist, or specialist you see that you're taking a blood thinner. This piece of information is vital before any medical or dental procedure, even a routine cleaning, as they might need to take special precautions.
Adopting healthy lifestyle choices is another powerful way to support your heart. For some, this includes looking at how alcohol might affect your heart health and interact with your medication. You can explore the life-changing benefits of quitting alcohol for overall wellness to learn more.
Making other positive shifts in your daily habits can also make a huge difference. For more ideas, you might find our guide to atrial fibrillation lifestyle changes helpful. With a solid routine and a bit of awareness, you can manage your treatment with confidence and keep enjoying your life.
Using Technology to Partner in Your AFib Care
It’s easy to feel like your health is something that only happens inside a doctor’s office. But in today's world, you have powerful tools right on your wrist that can make you an active partner in managing your AFib. This isn't about replacing your doctor; it's about making your conversations with them smarter and more productive.

Personal devices, especially smartwatches with electrocardiogram (ECG) functions, have become a game-changer for people living with AFib. They give you a way to capture exactly what your heart is doing, right in the moment you feel a symptom. This isn't just a neat feature, it’s a valuable piece of your personal health puzzle.
Turning Data Into a Clear Story
One of the key things your doctor wants to understand is your "AFib burden." This is simply a term for how much time your heart actually spends in an irregular rhythm. Is it a few fleeting minutes a week, or are you in AFib for several hours a day? The answer to that question can make a huge difference in treatment decisions, especially when it comes to blood thinners for AFib.
This is where your wearable device becomes your ally. By tracking episodes over time, you can stop saying things like, "I felt a bit funny last Tuesday," and instead show your doctor a clear record of exactly what your heart was doing and for how long.
This technology transforms you from a passive patient into an informed advocate for your own health. The data you collect helps build a more complete and accurate picture, ensuring your treatment plan is truly based on your experience.
Having a reliable way to monitor your heart rhythm is incredibly important. If you’re curious about how these devices work, you can learn more about if an Apple Watch can detect AFib in our detailed guide.
Making the Most of Your Wearable ECG
Just owning a smartwatch isn't enough; the real power comes from knowing how to use it effectively. You can learn to turn those squiggly lines and numbers into a clear, compelling story that your cardiologist can act on.
Here’s how to make your device a true partner in your care:
- Take ECGs During Symptoms: The moment you feel palpitations, lightheadedness, or shortness of breath, take a recording. This gives your doctor concrete evidence of what your heart was doing at that exact moment.
- Keep a Simple Log: Jot down what you were doing when the symptoms started. Were you exercising, feeling stressed, or just sitting on the couch? This context can help uncover potential triggers for your AFib.
- Share Your Reports: Most device apps let you create a PDF of your ECGs. It's a great idea to send these to your doctor's office before your appointment so they have time to review them.
Following these simple steps ensures that your appointments are as productive as possible. Instead of trying to rely on memory, you arrive with objective data in hand, ready to have a meaningful conversation. This partnership between you, your doctor, and your tech is a powerful way to manage your AFib with confidence.
How to Have a Confident Talk with Your Doctor
Making sure you and your doctor are on the same page is a huge part of managing your heart health. This is especially true when you're weighing a new treatment plan or just have questions that need answers. Your voice is critical in this process.
The best way to feel confident, not confused, is to prepare before your appointment.
This isn’t about second-guessing your doctor. It's about working together. The goal is what healthcare experts call shared decision-making, where you and your doctor become a team, choosing the best path forward for you. When it comes to your health, there's no such thing as a bad question.
Questions to Bring to Your Appointment
Walking into your appointment with a list of questions can completely change the dynamic. It shows you’re an active partner in your own care and helps make sure the conversation covers what matters most to you.
Here are a few straightforward questions you might ask about blood thinners for AFib:
- Could you walk me through why this specific medication is the right choice for me over others?
- What are the most common side effects I should keep an eye out for?
- Are there any specific warning signs that would mean I need to call you right away?
- Should I make any lifestyle changes while I'm on this medication?
A prepared conversation is a powerful one. It helps you build a partnership with your doctor, ensuring your treatment plan aligns with your health needs and your personal comfort level.
How to Express Your Concerns
If you're feeling nervous or unsure about a treatment, it’s really important to speak up. Voicing your concerns in a constructive way can lead to a much more productive conversation and build a stronger, more trusting relationship with your doctor.
For example, instead of a blunt statement like, "I don't want to take this," you could try framing it differently. Something like, "I'm feeling anxious about the risk of bleeding. Can we talk more about what that actually looks like in daily life?" This phrasing opens up the discussion and focuses it on finding a solution together.
Ultimately, being prepared helps you take an active role in your care. A good conversation should leave you feeling secure and in control of your health journey.
Common Questions and Honest Answers About Blood Thinners
It's completely normal to have questions as you start this journey. Let's walk through some of the most common things people wonder about when it comes to blood thinners for AFib, with clear, straightforward answers to give you peace of mind.
Will I Be on Blood Thinners for the Rest of My Life?
For most people with atrial fibrillation, taking a blood thinner is a long-term commitment. Think of it this way: the underlying risk of stroke from AFib doesn't just disappear, even on days you feel perfectly fine or when your symptoms are rare. The medication acts as a continuous shield, protecting your brain around the clock.
Of course, your doctor will regularly review your health with you. Your treatment plan isn't set in stone. If your health changes significantly down the road, it will absolutely be reassessed. The decision always comes down to balancing the powerful benefit of preventing a stroke against any potential risks of bleeding.
Can I Drink Alcohol While Taking a Blood Thinner?
This is a really important conversation to have directly with your doctor. For some people, moderate alcohol consumption might be okay, but it truly depends on your specific situation. Heavy drinking is a different story, as it can increase your bleeding risk and may interfere with how some blood thinners work, especially warfarin.
Your doctor can give you personalized advice based on the exact medication you’re on, your overall health, and your lifestyle. Being open and honest here is key. It helps your doctor give you the safest guidance possible.
Your health plan is a partnership. Openly discussing your lifestyle, including alcohol use, allows your doctor to provide the best and safest guidance tailored just for you.
Are There Natural Alternatives to Prescription Blood Thinners?
It's understandable to be cautious about medications and look for more "natural" solutions. You may have heard that some foods and supplements (like turmeric or fish oil) have mild blood-thinning properties. While that's true to a small degree, they are not a safe or effective substitute for prescription medications for AFib.
The stroke risk that comes with AFib is serious, and prescription anticoagulants are the only treatments that have been proven through extensive, rigorous research to dramatically lower that risk. Trying to rely on unproven alternatives can leave you unprotected when you need it most. Always talk to your doctor before starting any new supplement, as many can have unexpected and sometimes dangerous interactions with your prescribed medication.
Our expert-reviewed ECG service helps you monitor your heart rhythms with confidence, turning wearable data into clear insights you can share with your doctor.










.png)
.png)