Key Takeaways
Pregnancy is an incredible and transformative journey, filled with many changes to support your growing baby. One of the most important changes happens in your cardiovascular system. These natural adjustments can sometimes show up on your ECG, and while most of them are completely normal, they can be confusing or even concerning without context.
Cardiovascular Adaptations in Pregnancy
During pregnancy, your body undergoes a series of cardiovascular adjustments to meet the increased demands of both mother and baby. These changes begin early in the first trimester and continue to progress throughout the pregnancy, reaching their peak in the third trimester.
Key cardiovascular adaptations include:
- Increased Blood Volume: Your total blood volume can increase by 30-50%, leading to a greater workload for your heart.
- Increased Cardiac Output: The amount of blood your heart pumps per minute increases significantly (by 30-50%) to ensure adequate blood flow to the uterus, placenta, and other organs.
- Increased Heart Rate: Your resting heart rate typically increases by 10-20 beats per minute.
- Decreased Systemic Vascular Resistance: Blood vessels relax to accommodate the increased blood volume, leading to a slight decrease in blood pressure in early to mid-pregnancy.
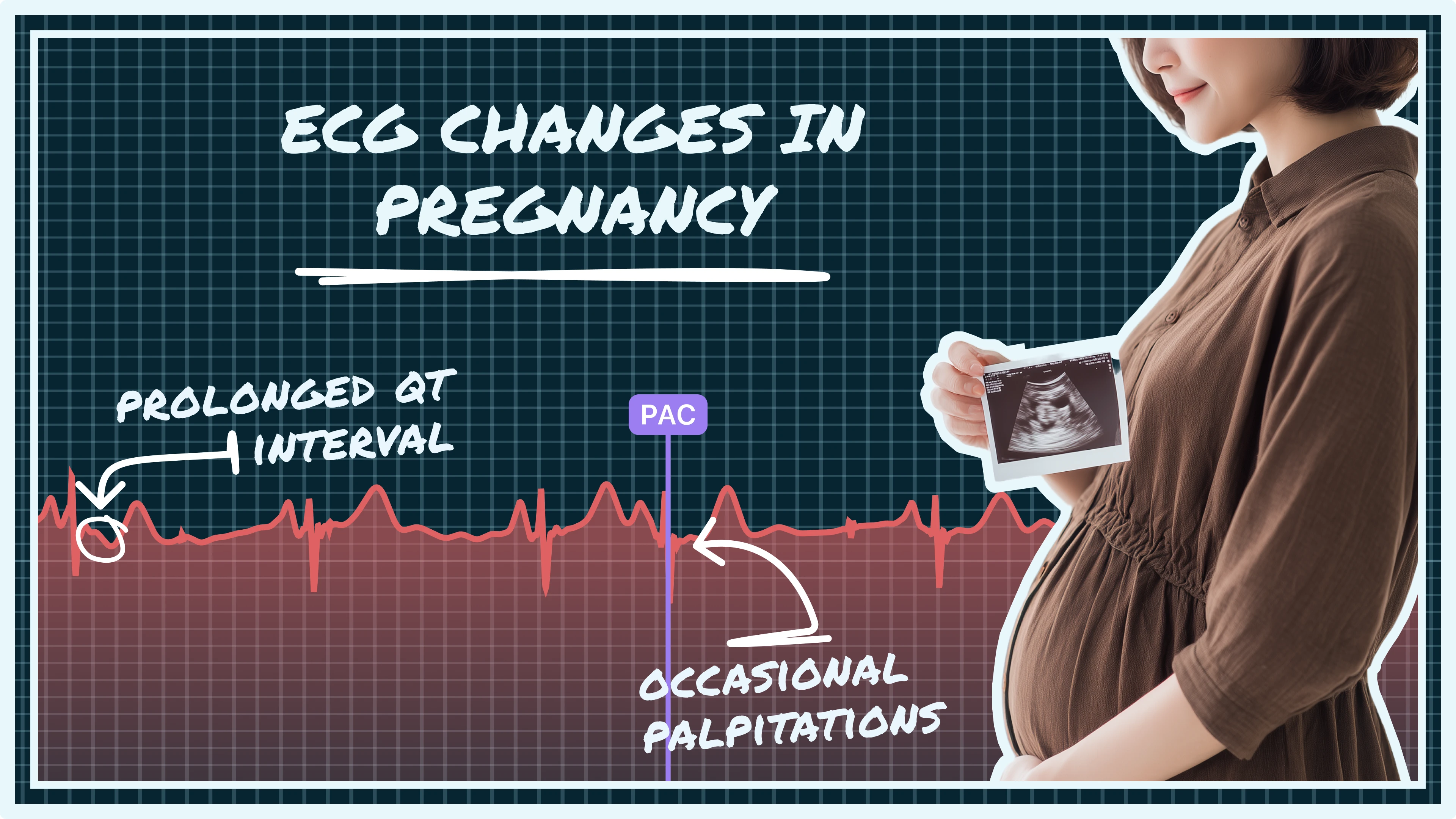
Normal ECG Findings in Pregnancy
These physiological changes are normal and necessary, but they can lead to alterations in your ECG that might be misinterpreted if the context of pregnancy is not considered. Understanding these normal variations is key to avoiding unnecessary concern.
Common normal ECG findings in pregnant women include:
- Sinus Tachycardia: A slightly faster-than-usual heart rate (typically over 100 bpm) that reflects your body’s increased need for oxygen and circulation during pregnancy.
- Left Axis Deviation: A harmless shift in the heart’s electrical axis due to the growing uterus pushing the heart slightly to the left.
- Nonspecific ST-T Wave Changes: Minor changes in the shape of ST segments and T waves that are common and not usually a cause for concern.
- Increased QRS Voltage: Stronger electrical signals from the heart that can occur due to the increased blood volume and enhanced cardiac workload.
- Shortened PR and QT Intervals: A reflection of the overall faster electrical conduction and heightened metabolism in pregnancy, typically within normal limits.
It's important for healthcare providers to be aware of these normal pregnancy-related ECG changes to avoid misdiagnosing a healthy pregnant woman with a cardiac condition.
Heart feels off during pregnancy? Qaly experts review your ECGs and help you understand what’s going on.









.png)
.png)