Key Takeaways
Hello Heart Hero. It can be truly frightening when your heart suddenly starts racing or skipping beats right after a meal or during a bout of indigestion. Rest assured, you're not alone in this experience, and it's certainly not just in your head. The connection between your stomach and your heart is very real, and understanding it is the first step toward finding peace of mind.
Why Your Stomach Can Upset Your Heart
That fluttering or pounding sensation you feel is often a direct result of what’s happening in your digestive system. Think of your stomach and heart as close neighbors who share a very sensitive communication line.
When one neighbor is having a noisy, disruptive party (like your stomach dealing with gas, bloating, or acid reflux), the other neighbor (your heart) is bound to hear the commotion and get unsettled. This is the essence of the link between indigestion and heart palpitations.
This connection isn't just a hunch; it’s a well-documented physiological response. In fact, a recent meta-analysis of over 500,000 people found that individuals with frequent indigestion were 30% more likely to report experiencing heart palpitations than those without digestive issues. It’s a surprisingly common link.
The Gut-Heart Connection Explained
So, what exactly is going on in there to cause this reaction? It mostly comes down to a shared nerve pathway and the simple fact that your organs are packed in closely together. When your stomach is upset, it can set off a chain reaction in a few ways:
- Pressure and Irritation: A stomach filled with gas or excess acid can physically push up against the diaphragm. This pressure can irritate the heart muscle and the nerves around it, sometimes causing it to beat irregularly.
- Nerve Signals: The vagus nerve is a major communication highway connecting your brain, heart, and digestive tract. When your stomach is irritated, it can send "stress" signals up this nerve, which can directly throw your heart's rhythm off-kilter.
- Chemical Responses: The body's reaction to certain foods or even stress can release adrenaline, which naturally speeds up your heart rate. If your digestive system is already acting up, this response can feel much more intense.
This intricate relationship is often called the gut-heart axis. Recognizing that a digestive issue can create a cardiac symptom is key to managing the anxiety that often comes with palpitations.
This understanding helps shift the focus from fear about your heart to curiosity about your gut. For many, anxiety itself can be a major trigger, creating a vicious cycle where worry about the heart worsens digestive symptoms, and vice-versa. It’s helpful to explore if anxiety might be contributing to your arrhythmia concerns.
To go a bit deeper, learning about how your digestive system influences your overall well-being is a powerful tool. A great place to start is understanding the gut-brain axis, which plays a huge role in this entire process.
The Vagus Nerve: Your Body's Information Superhighway
To really understand why a grumpy stomach can make your heart do a little dance, we need to talk about one of the most amazing parts of your body: the vagus nerve.
Picture it as a massive, sensitive information superhighway. It runs directly from your brain stem down through your chest and into your major organs, including your stomach and, crucially, your heart.
It's the main line of communication for your body’s “rest and digest” system, which helps manage everything from your heart rate and digestion to your mood. Because this nerve physically connects both your stomach and your heart, these two organs are in constant communication. This direct link is the key to understanding the connection between indigestion and heart palpitations.
How Stomach Issues Can Trigger Heart Symptoms
When your digestive system is humming along nicely, the signals traveling up and down the vagus nerve are smooth and orderly. But when you get indigestion, bloating, or acid reflux, your stomach gets irritated.
This irritation is like sending a blast of static down the line. It creates chaotic or overly strong "alert" signals that shoot right up the vagus nerve.
Your brain and heart can misinterpret this digestive distress as a genuine emergency. In response, the vagus nerve might momentarily mess with your heart’s normal electrical rhythm. The result? That scary sensation of a skipped beat, a flutter, or a sudden racing pulse. It isn't a problem with your heart itself, but more like a crossed signal from its very close neighbor, the stomach.
The infographic below shows a simple visual of this pathway, connecting indigestion to heart palpitations through this shared nerve.
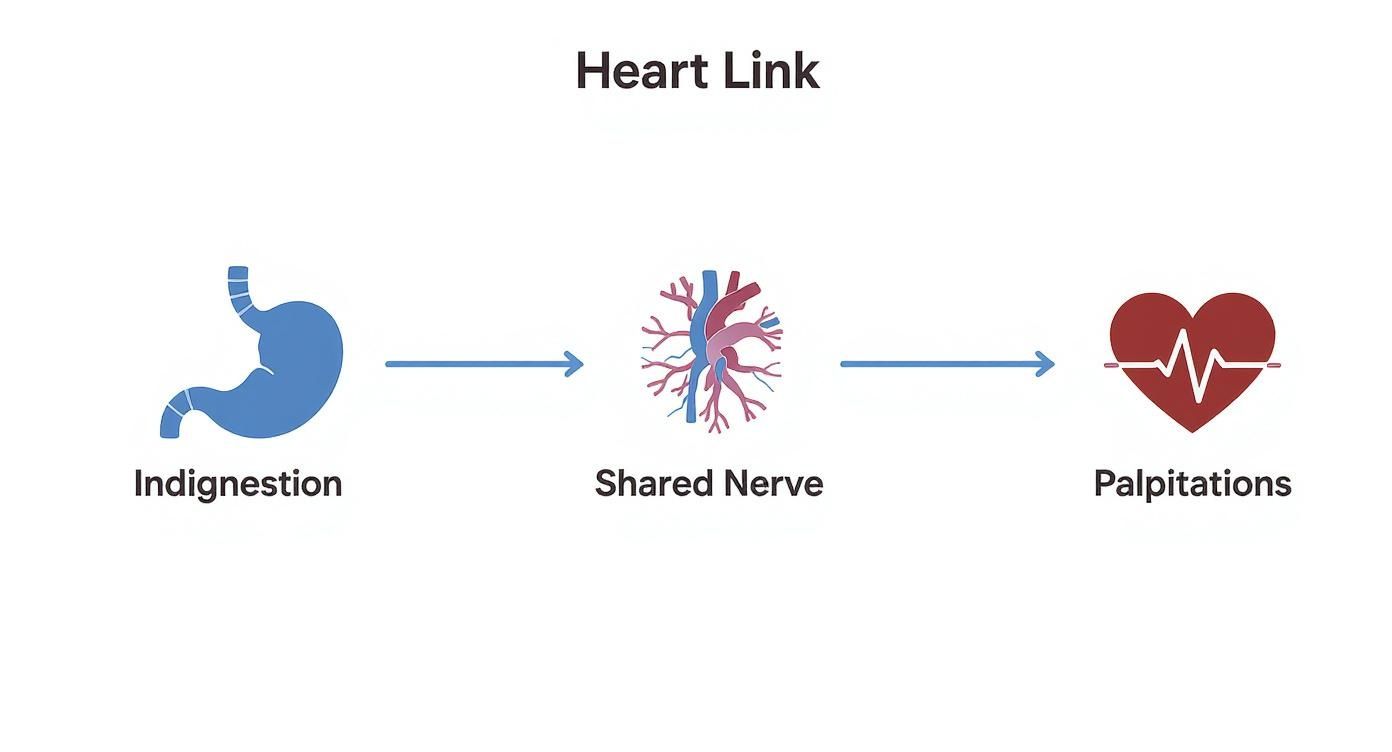
This visual makes it really clear how an issue that starts in the stomach doesn't just stay there. It can travel up a nerve and directly influence how your heart behaves.
Why Is This Knowledge So Reassuring?
Understanding the vagus nerve's role here is incredibly empowering. It takes the experience from being a scary, random event and turns it into something you can actually understand: a predictable biological response.
Knowing that your palpitations could be a simple case of nerve irritation from your gut can significantly reduce the anxiety that often makes these episodes feel so much worse.
Instead of jumping to the worst-case scenario about your heart, you can start connecting the dots back to your digestive health. You might start noticing patterns, like palpitations that only seem to pop up after a particularly large, spicy, or fatty meal.
This shift in perspective is the first and most important step toward regaining a sense of control over your body. It allows you to focus on the root cause in your stomach, rather than just worrying about the symptom in your chest. And that can bring some much-needed peace of mind.
We've explored the fascinating connection between your gut and your heart. Now, let's get specific and meet the two most common culprits behind that frustrating mix of indigestion and heart palpitations.
Is It GERD or Roemheld Syndrome Causing Palpitations?
Knowing the specific mechanics can be a huge help in figuring out what might be happening in your own body. We're going to look at two conditions that are often responsible for this annoying symptom: GERD and Roemheld Syndrome.
While both involve your digestive system throwing your heart's rhythm off-kilter, they work in slightly different ways. By learning to spot their unique signs, you can start connecting your own experiences to a potential cause.
GERD: The Chemical Irritant
You've probably heard of GERD, or Gastroesophageal Reflux Disease, as just really bad heartburn. But its impact can go way beyond a simple burning feeling in your chest.
With GERD, stomach acid flows backward, creeping up into your esophagus. This tube runs right behind your heart, nestled in very close proximity to that vagus nerve we talked about earlier.
When that harsh acid splashes into this sensitive area, it's like a chemical irritant setting off an alarm. This irritation can directly provoke the vagus nerve, sending those scrambled, chaotic signals that lead straight to heart palpitations. You might notice this more after certain trigger foods or when you lie down at night, since gravity is no longer helping to keep the acid in its place. In fact, many people report feeling heart palpitations after eating certain meals, which is a classic sign of this gut-heart connection.
Roemheld Syndrome: The Physical Pressure
A less-known but equally important condition is Roemheld Syndrome. Think of this one as a problem of physical pressure, not chemical irritation.
This syndrome happens when a ton of gas gets trapped in your stomach and intestines. This buildup can cause some serious bloating, pushing your diaphragm upward and physically pressing against your heart.
This pressure can literally interfere with your heart's ability to beat normally. It can also, once again, stimulate that all-important vagus nerve, triggering palpitations from the sheer force of the bloating.
Roemheld Syndrome perfectly illustrates how a purely digestive issue like trapped gas can create a very real and alarming cardiac symptom. It’s not "all in your head"; it's a physical phenomenon.
This condition, also known as gastrocardiac syndrome, is finally getting more attention for its role in otherwise unexplained heart flutters. Clinical observations suggest that up to 20% of patients with mysterious palpitations might actually have underlying digestive issues like indigestion and bloating. By understanding these two very different causes, you can become a better detective of your own body's signals.
When to Worry and When to Find Calm
It's completely normal for your mind to jump to the worst-case scenario when you feel your stomach acting up and your heart doing flip-flops at the same time. The biggest question is always, "Is this dangerous?" That's a valid concern, and our goal here is to give you some clarity.
Knowing how to tell the difference between a harmless, digestion-related flutter and something more serious is a powerful tool. It helps you stay calm and make the right call, especially if you're hesitant to run to the doctor for every little thing.
Most of the time, palpitations tied to indigestion are temporary and nothing to worry about. They often follow a pretty predictable pattern. For instance, you might notice they pop up right after a big meal, last only a short time, and then fade away as your stomach settles down.
Red Flags You Should Never Ignore
While most cases are linked to your gut, it’s critical to know the signs that point to a potential heart issue. Your heart is too important to guess about.
Think of the following symptoms as a simple but non-negotiable mental checklist. If your palpitations show up with any of these, it's time to seek immediate medical attention:
- Severe Chest Pain or Pressure: This isn’t the familiar burn of heartburn. It can feel like a squeezing, tightness, or a heavy weight sitting on your chest.
- Dizziness or Fainting: Feeling lightheaded, like you might pass out, or actually fainting is a major red flag.
- Significant Shortness of Breath: If you’re struggling to catch your breath and it’s not from physical effort, pay close attention.
- Pain Radiating to Other Areas: Discomfort that spreads to your arm, neck, jaw, or back is a classic warning sign.
Trust your intuition. If the palpitations feel intensely wrong, last for a long time without stopping, or come with a general sense of doom, it is always better to be safe and get checked out.
For a more detailed breakdown, understanding when to see a doctor for heart palpitations can provide extra clarity and peace of mind.
The GERD and Atrial Fibrillation Connection
It's also worth knowing about the proven link between chronic indigestion and certain heart rhythm conditions. For example, research has uncovered a notable association between GERD and atrial fibrillation (Afib), a common type of irregular heartbeat.
Studies have found that up to 14% of people with GERD also had Afib. That's a pretty significant number when you compare it to the 1% to 2% prevalence in the general population.
This doesn't mean your indigestion is causing Afib, but it does highlight why paying attention to these connected symptoms is so important for your long-term health. Learning to spot the difference between a simple flutter and a red-flag event is your first step toward managing both your digestion and your heart with confidence.
Practical Steps to Calm Your Stomach and Heart
Knowing the why behind your symptoms is a great first step, but the real power comes from taking practical, gentle steps to find relief. This isn't about some drastic, stressful overhaul of your life. Instead, think of it as building a personal toolkit of small, sustainable habits that can make a huge difference for both your gut and your heart.
For many people, regaining a sense of calm starts with what’s on their plate. You don’t have to be a nutritionist. Just becoming a bit of a detective with your own diet is the first move in managing the link between indigestion and heart palpitations.
Identify Your Personal Triggers
Your body has its own unique rulebook. A food that’s perfectly fine for someone else might be a major trigger for you. The key is to start paying close attention to how you feel after eating certain things.
Some of the usual suspects include:
- Spicy or Acidic Foods: Think hot sauces, citrus fruits, and tomatoes. These can ramp up stomach acid production, leading straight to reflux.
- Large, Fatty Meals: These are tough to digest. They force your stomach to work overtime producing acid and can lead to bloating that physically presses on your diaphragm.
- Caffeine and Alcohol: Both are well-known stimulants that can directly mess with your heart rate, on top of irritating your digestive system.
Try keeping a simple food and symptom journal for a week or two. You might be surprised by the patterns that pop up. Just jot down what you ate, when you ate it, and if any palpitations showed up afterward.
Adjust Your Eating Habits
It’s not just what you eat, but how you eat. Making a few simple adjustments can prevent your stomach from getting overwhelmed, which in turn helps keep your heart calm and steady.
Here are a few gentle strategies to try:
- Eat Smaller, More Frequent Meals: Instead of three big meals, try five or six smaller ones. This simple change keeps your stomach from getting too full and distended, cutting down the risk of both acid reflux and that physical pressure on your heart.
- Stay Upright After Eating: Gravity is your best friend here. Make it a rule to avoid lying down for at least two to three hours after a meal. This helps keep stomach acid where it belongs and can be a game-changer if your palpitations tend to act up at night.
The goal is to work with your digestive system, not against it. By giving it less work to do at any one time, you reduce the chances of it sending distress signals that upset your heart's rhythm.
Finally, never underestimate the mind-gut connection. Stress and anxiety flood your body with adrenaline, a hormone that can throw fuel on the fire of both indigestion and heart palpitations, locking you in a frustrating cycle.
Many people find incredible relief by actively managing their stress. Explore different strategies for reducing stress naturally to see what clicks for you. Even something as simple as a deep breathing exercise of inhaling slowly for four counts and exhaling for six can calm your entire nervous system in just a few minutes.
Using Wearable ECGs for Peace of Mind

It’s one thing to know that indigestion and heart palpitations are linked, but it’s another thing to experience it. In a world where getting clear health answers can feel like a frustrating waiting game, today’s technology can be an incredibly powerful ally.
The uncertainty is often the worst part. But you no longer have to just guess what's going on when you feel that flutter or pound after a heavy meal.
Modern tools, like the ECG function on your smartwatch, were practically made for these situations. They give you the power to capture your heart's electrical rhythm the very moment you feel symptoms.
Gathering Your Own Data
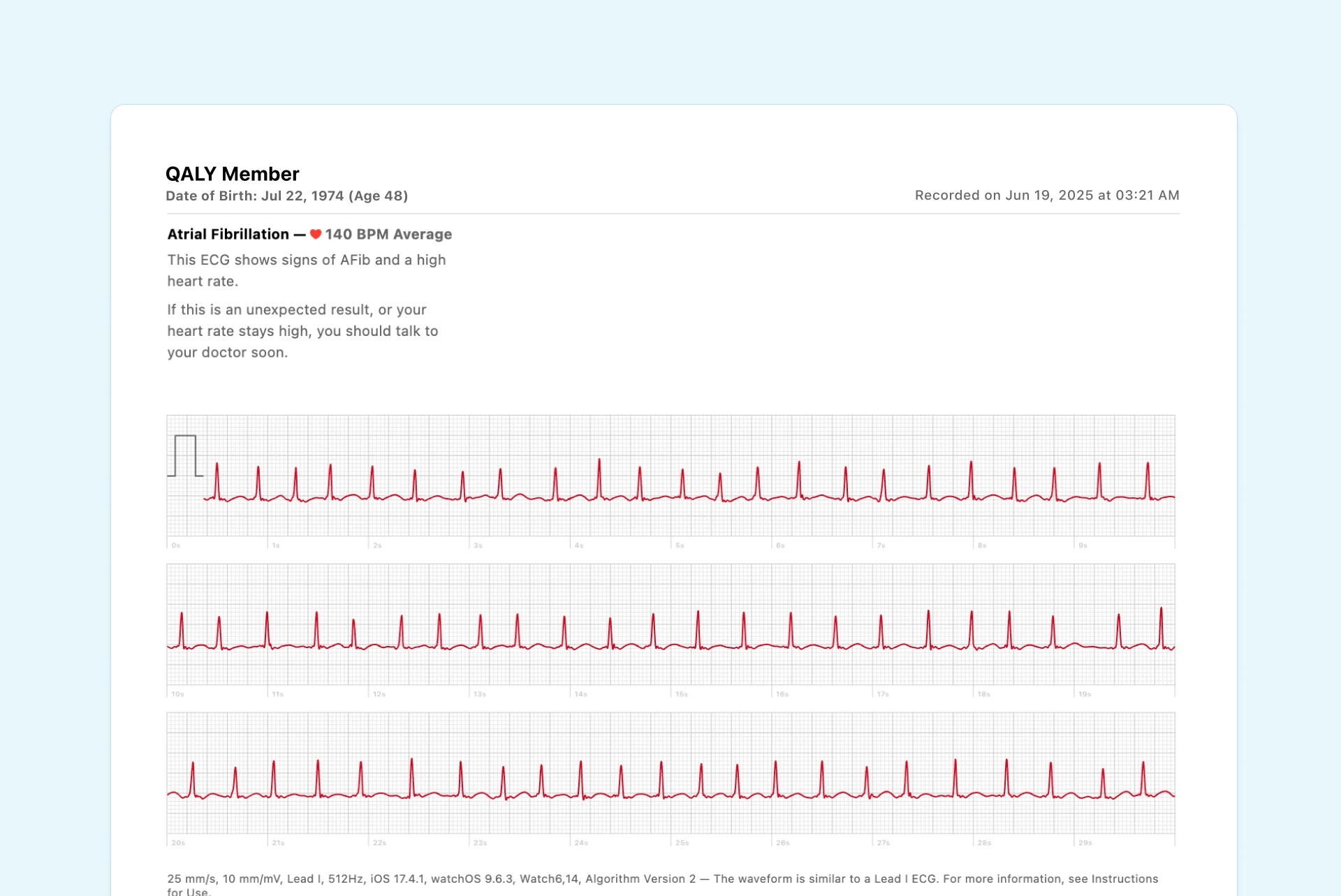
Think of your smartwatch as your personal heart health detective. The next time you feel a strange sensation, you can take a quick ECG recording. This isn’t about diagnosing yourself. You should never do that. It's about collecting valuable, real-time evidence.
Having a recording of your heart's activity during an episode is a game-changer. It shifts the conversation from, "Doc, I felt a weird flutter last Tuesday," to, "Here is exactly what my heart was doing when I felt that flutter."
This simple action moves you from a place of fear and uncertainty to one of proactive monitoring. You're no longer just a passive worrier; you become an active partner in your own healthcare.
That recording gives you and your doctor a concrete place to start the conversation, armed with actual data.
Making Doctor's Visits More Effective
When you capture an ECG during palpitations after eating, you're helping connect the dots between your digestion and your heart. This kind of information makes it much easier to spot patterns.
Is it a benign issue like vagus nerve irritation, or is it something that needs a closer look? The data helps answer that question.
These devices bridge the gap between your appointments. By using a portable electrocardiogram monitor, you can gather the specific insights needed for a focused, data-driven discussion with your doctor. And that ultimately leads to real answers and greater peace of mind.
Common Questions About Indigestion and Palpitations
When you're dealing with something as unsettling as heart flutters after a meal, it's natural to have questions. Let's clear up some of the most common concerns.
Can Trapped Gas Really Cause Heart Palpitations?
Yes, it absolutely can. It might sound strange, but there's a direct mechanical link. When a lot of gas gets trapped in your stomach, it can literally push your diaphragm upward, which in turn puts pressure on your heart.
This physical crowding, combined with signals sent through the vagus nerve (the superhighway connecting your gut and heart), can be enough to knock your heart's rhythm off-kilter and trigger those thumps and flutters. This phenomenon is often called Roemheld Syndrome.
How Long After Eating Can Palpitations Start?
There's no single timeline here; it really depends on your body and your digestive system.
Some people feel that flutter within minutes of finishing a big meal, as their stomach starts to stretch and the digestive process kicks into high gear. For others, it might be 30 minutes to a few hours later, especially if digestion is sluggish or if GERD is part of the picture. This is particularly common when lying down, which can allow stomach acid to creep up and irritate the esophagus, further aggravating the vagus nerve.
Trust your body. While these symptoms are often harmless, they're your body's way of telling you something is off. Don't ignore the signals.
Should I Go to the ER for Palpitations After Eating?
Most of the time, flutters tied to a big meal aren't a medical emergency. But it's critical to know the difference between a benign flutter and a true red flag.
You should head to the ER immediately if your palpitations come with any of these symptoms:
- Severe chest pain or a feeling of intense pressure
- Dizziness, lightheadedness, or fainting
- Significant shortness of breath
If your palpitations are brief, seem clearly connected to eating, and go away on their own without these other symptoms, it's usually safe to schedule a non-urgent visit with your doctor to get to the bottom of it.
Stop wondering what your heart is doing during those unsettling moments. With Qaly, you can get your at-home ECGs analyzed by certified experts in minutes.










.png)
.png)