Key Takeaways
Flecainide is a powerful antiarrhythmic medication prescribed to manage irregular heart rhythms. But like any medicine that works on the heart, it comes with potential side effects that can range from mild dizziness to more serious heart-related issues.
Getting familiar with what to expect is the best first step you can take toward safely managing your heart health while on this treatment.
Hello Heart Hero: A Guide to Starting Flecainide
If you're reading this, chances are you or someone you care about is about to start taking flecainide. It's totally normal to feel a mix of hope for a steady heartbeat and a little nervousness about what's next. Think of this guide as a calm, clear conversation starter, designed to answer your questions with straightforward information.
We get it. You might feel a bit wary about adding another prescription to your daily routine, especially when you're skeptical about the healthcare system. Our goal is to give you the knowledge you need to be an active partner in your healthcare, not just a passive recipient.
What Is Flecainide and Why Is It Used?
Flecainide works directly on your heart’s electrical system. Imagine the electrical pathways in your heart are like tiny highways. In conditions like atrial fibrillation (AFib), the traffic on these highways gets chaotic, leading to an irregular and often rapid heartbeat.
Flecainide acts like a skilled traffic controller. It slows down the electrical signals to bring order and stability back to your heart's rhythm.
It’s most often prescribed for specific types of arrhythmias, such as:
- Paroxysmal Atrial Fibrillation (PAF), where episodes of irregular heartbeats start and stop on their own.
- Ventricular Arrhythmias, which are serious rhythm problems that start in the heart's lower chambers.
By getting these conditions under control, the goal of flecainide is to dial back symptoms like palpitations, shortness of breath, and fatigue, helping you get back to a better quality of life.
Starting a new heart medication is a big step. The key isn’t to fear the side effects of flecainide, but to understand them. Knowing what’s a minor adjustment versus what needs immediate attention is the most powerful tool you have.
Preparing for Your Journey with Flecainide
Finding the right treatment path is a partnership between you and your doctor. Before you start, your doctor will likely run several tests, including an electrocardiogram (ECG), to make sure flecainide is a safe choice for your specific heart condition. This careful screening is crucial.
Once you begin, ongoing observation is part of the process. For more on this, check out our detailed guide on what is cardiac monitoring to see how technology helps keep you safe.
Throughout this article, we'll walk you through everything from the common side effects that often fade over time to the serious signs you should never ignore. You're in the right place to get informed and feel more confident.
The Study That Reshaped Flecainide Safety
To really get why your doctor is so careful with flecainide, we need to take a quick trip back in time.
Understanding this medication's history isn't just for trivia night; it’s the key to feeling confident and in control of your treatment plan today. The modern story of flecainide’s safety was almost entirely written by one groundbreaking medical study.
This wasn't just any old research project. It was a landmark event in cardiology called the Cardiac Arrhythmia Suppression Trial, or CAST. Before this trial, the thinking was pretty simple: if irregular heartbeats after a heart attack are a bad sign, then using a powerful drug to stop them should save lives. It seemed perfectly logical at the time.
So, researchers set out to prove it. The goal was to show that medications like flecainide could prevent deadly arrhythmias in people who had recently survived a heart attack, offering protection to a very vulnerable group.
What Researchers Discovered
The medical community was hopeful, but the results were the opposite of what everyone expected. In fact, they were so alarming they sent shockwaves through the field of cardiology.
The study had to be stopped early because of what it revealed about the side effects flecainide could cause in this specific group of patients.
Instead of saving lives, the trial showed that flecainide and a similar drug actually increased the risk of death for patients who had structural heart damage from a previous heart attack. This was a jaw-dropping discovery, and it taught doctors an invaluable lesson that has shaped heart rhythm treatment ever since.
Essentially, the study found that for this particular group, the very act of suppressing minor, less threatening irregular heartbeats could, tragically, trigger much more dangerous ones.
The Critical Findings of CAST
The findings were so significant that they led to an immediate change in the prescription of these drugs. Data published in 1991 showed that patients taking flecainide had a 2.5 times higher death rate compared to those given a placebo.
In the group taking flecainide, the death rate was 5.6%.
In the placebo group, the death rate was only 2.3%.
This was a difference no one could ignore, and it led directly to the strong warnings you see tied to the drug today. You can dive deeper into the detailed analysis from the National Institutes of Health to see the data that reshaped flecainide’s use.
Now, this history might sound scary, but it's really a story about modern medical safety. It’s precisely why your doctor ordered a thorough check of your heart's structure, likely with an echocardiogram, before even thinking about this medication for you.
The lesson from CAST wasn't that flecainide is a "bad" drug. The real takeaway was that it's a powerful tool that must be used only for the right patient, in the right situation. Your prescription today is based on decades of learning exactly who that patient is.
Why This History Matters for You
Knowing this backstory is empowering. It explains the "why" behind your doctor's cautious and personalized approach.
The strict rules for prescribing flecainide today are a direct result of the hard lessons learned from CAST. Doctors now know with certainty that while it's a safe and highly effective option for people with structurally normal hearts, it should be avoided in those with conditions like coronary artery disease or a history of heart attack.
This is a perfect example of how medicine learns, evolves, and ultimately becomes safer for patients. Your healthcare team is standing on the shoulders of this critical research, making sure that the potential side effects flecainide might have are carefully weighed against its benefits for your specific heart. For a broader look at how different heart rhythm medications work, you might find our guide on understanding antiarrhythmic drugs and their side effects helpful.
Understanding Common Non-Cardiac Side Effects
When you start any new medication, it’s a bit like your body is meeting someone new. It takes a little time to adjust and figure out how to work together. So, it's completely normal to feel a bit "off" at first, and flecainide is no different.
While we often focus on the heart-related effects, many of the initial side effects of flecainide aren't directly cardiac. These sensations can be unsettling, but knowing what they are and why they happen is the first step toward feeling more in control. The good news is that many of these are temporary and often fade as your body gets used to the medication.
Dizziness and Vision Changes
One of the most common things people report is a sense of dizziness or lightheadedness. You might also notice some visual disturbances, like blurred or even double vision.
This happens because flecainide, while working to calm your heart's electrical signals, can also influence nerve signals elsewhere in your body, including those connected to balance and sight. It's like your body's internal communication system is temporarily getting a new set of rules, which can make you feel wobbly, especially when you stand up or move suddenly.
To help manage this, try these simple tips:
- Move slowly and deliberately, especially when going from sitting or lying down to standing. Give your body a moment to catch up.
- Stay well hydrated all day. Dehydration can make dizziness feel much worse.
- Be cautious when driving or doing anything that requires sharp focus until you know how flecainide affects you.
These effects are often most noticeable right after you take a dose and typically become less intense over time.
Headaches and Stomach Upset
It’s also not unusual to get headaches or feel a bit of nausea when first starting flecainide. An upset stomach is a common reaction to many medications as your digestive system adapts. Headaches can pop up for similar reasons as dizziness, as the medication influences your central nervous system.
While they're an inconvenience, these side effects are usually mild. One practical tip is to take your flecainide dose with a meal or a small snack. This can help cushion your stomach and often reduces that nauseous feeling. If headaches stick around, let your doctor know, but they too often get better within the first couple of weeks.
A wide-ranging analysis confirmed that non-cardiac side effects are a known part of the flecainide experience. The study found that about 17% of patients taking flecainide reported issues like dizziness and vision changes, compared to 11% in a control group. The good news is that for the right patients, these events are typically manageable.
Practical Steps for Coping
Feeling different can be worrying, but remember that your body is simply adjusting. Most of these non-cardiac side effects are a sign that the medication is active in your system. They don't necessarily mean something is wrong.
If you experience any of these sensations, the best approach is to:
- Keep a simple log: Note what you feel, when it happens, and how intense it is. This information is incredibly helpful for your doctor.
- Stay in communication: Don't hesitate to call your doctor or pharmacist if a side effect is particularly bothersome or doesn't seem to be improving.
- Give it time: Be patient with your body. For many people, these initial hurdles smooth out within a few weeks.
Understanding the potential side effects of different antiarrhythmic medications can also provide valuable context. For instance, you can read our guide on the side effects of mexiletine, another drug used for heart rhythm disorders. This information helps you build a broader knowledge base for conversations with your healthcare team.
Serious Heart-Related Side Effects to Watch For
This is the topic that probably concerns you the most, so let’s walk through it with care and clarity. While the common, non-cardiac side effects are often just temporary annoyances, it’s the heart-related ones that need your full attention. The goal here isn't to scare you, but to empower you with knowledge.
Knowing what to look for and when to get help is the most important part of staying safe on this medication. These serious effects are less common, but being prepared is your best line of defense.
The main concern with any antiarrhythmic drug is a phenomenon called proarrhythmia. It’s a complicated-sounding word, but the meaning is simple: the very medication meant to fix an irregular heartbeat can sometimes trigger a new or even worse one. This is one of the key serious side effects of flecainide.
Think of your heart's electrical system like a perfectly timed orchestra. Flecainide is the conductor, brought in to quiet a section that's playing too fast. Usually, it restores harmony. But on rare occasions, the conductor's new tempo can unintentionally throw another part of the orchestra off-key, creating a different, and sometimes more dangerous, rhythm.
Understanding Proarrhythmia and Its Signs
This risk is exactly why your doctor did a thorough check of your heart's structure before ever writing the prescription. The famous CAST study taught us that this risk is highest in people with underlying structural heart problems. For those with structurally healthy hearts, the risk is much lower, but it’s never zero.
The most critical thing you can do is learn to recognize the warning signs that your heart's rhythm has changed for the worse. These aren't subtle hints; they're strong signals from your body that you need to listen to.
This decision tree infographic can help you quickly sort through common side effects.
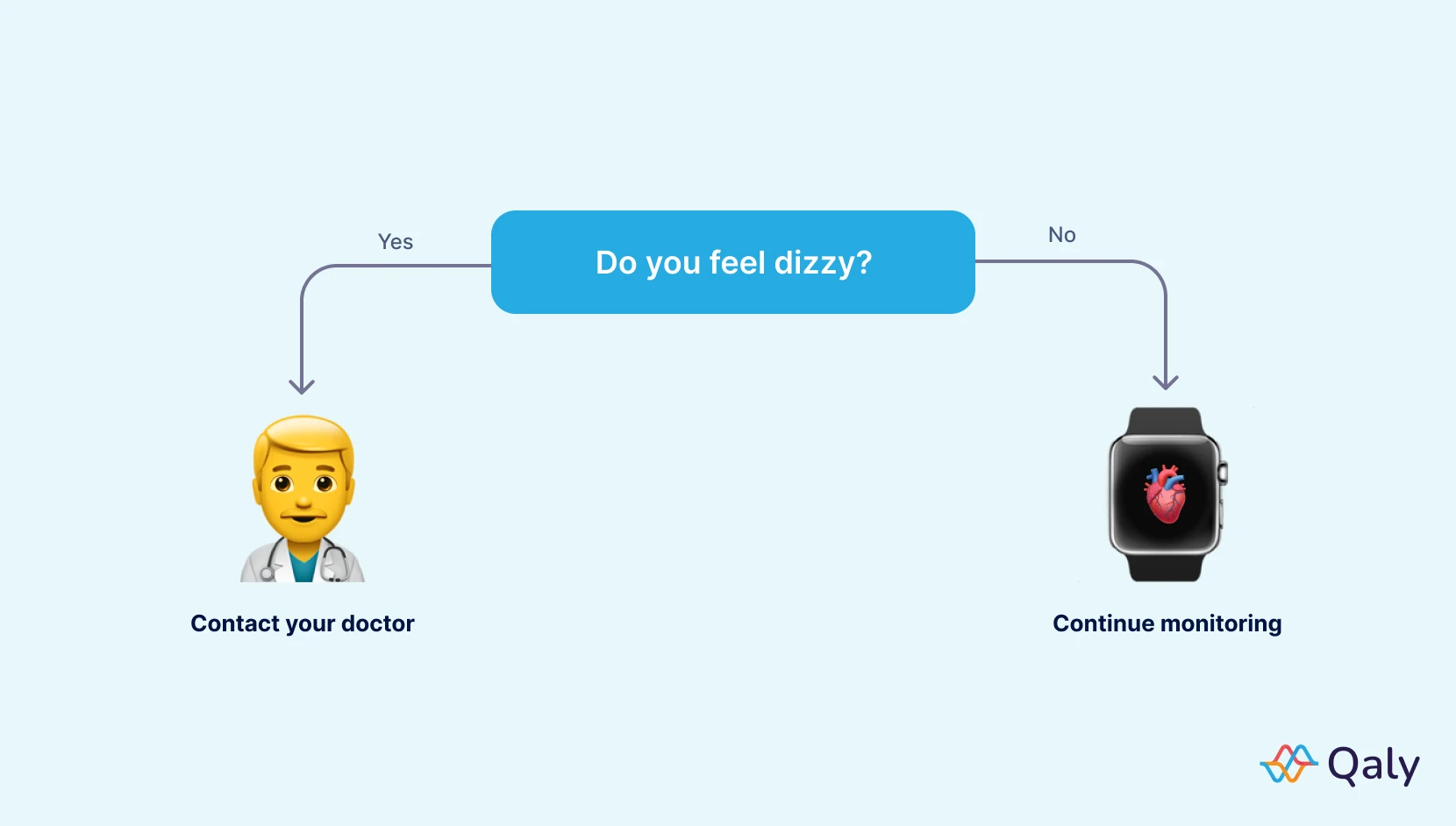
As the visual guide shows, common symptoms like mild dizziness warrant a conversation with your doctor, but you should continue to monitor your health as part of your routine.
On the other hand, key signs of a potential proarrhythmic event are much more serious and include:
- Fainting or feeling like you might faint. This is a major red flag that you should never ignore.
- Severe, sudden dizziness. This feels different and far more intense than the mild lightheadedness we talked about earlier.
- A new or dramatically different heartbeat. This could feel like a very fast, chaotic, or pounding sensation in your chest that doesn't go away.
- New or worsening shortness of breath. If you suddenly find yourself struggling to breathe during normal activities, it's a sign to seek help.
- Sudden chest pain. This always requires immediate medical attention.
Specific Changes to Your Heart Rhythm
Research has pinpointed the specific types of rhythm changes that can happen as a side effect of flecainide. For instance, one study found that among patients on a certain form of flecainide, the most reported proarrhythmic effects were a slow heart rate, or bradycardia (13.2%), and extra heartbeats from the lower chambers, called ventricular extrasystoles (10.6%).
If you experience any of these major warning signs, it is critical to contact your doctor immediately or seek emergency medical help. This isn't a "wait and see" situation. Acting fast is key to staying safe.
Flecainide works by directly affecting certain intervals in your heart's electrical cycle, which are visible on an ECG. It intentionally widens the QRS interval and can sometimes prolong the QT interval. While some QRS widening is expected and even desired, too much can become a problem. That’s why your doctor will keep a close eye on your ECG. If you want to dive deeper into this, our article on drugs that cause QT prolongation provides more helpful context.
To get a better sense of the bigger picture, you might also explore information on similar antiarrhythmic medications like Amiodarone. Understanding how different drugs work can help you have more informed discussions with your doctor about your treatment plan. Being an educated partner in your own healthcare is one of the most powerful things you can do.
How Flecainide Interacts with Other Factors
Your body is a remarkable and complex ecosystem. Think about it like this: starting a medication like flecainide doesn't happen in a vacuum. It's like adding a new, powerful plant to a finely-tuned garden. It will interact with everything else already there.
This includes other medications, supplements, and your own unique health conditions. Understanding these interactions isn't about memorizing a long list of rules. It’s about seeing why it’s so critical to be completely open with your healthcare team. They're the expert gardeners who can make sure everything in your system works together safely and effectively.
When Medications Cross Paths
One of the most important things to watch for is how flecainide gets along with other medications you're taking. Imagine it like a busy highway. Some medications use the same "lanes" in your body as flecainide, and this can cause traffic jams, making its effects much stronger or weaker.
This is especially true for drugs that are processed by the same pathways in your liver. Flecainide is mostly handled by a specific liver enzyme called CYP2D6. When another drug is competing for this enzyme's attention, it can cause the levels of flecainide in your blood to rise, increasing the risk of side effects.
Here are some common types of medications that need careful management when you're taking flecainide:
- Other heart rhythm drugs: Combining antiarrhythmics can have a powerful, and sometimes unpredictable, effect on your heart's electrical system.
- Certain antidepressants: Many common antidepressants, especially SSRIs, also use that same CYP2D6 pathway.
- Specific antibiotics and antifungals: Some of these can slow down how fast your body breaks down flecainide, making it build up.
- Beta-blockers and calcium channel blockers: While often used together, your doctor will need to monitor this combination very closely.
This is exactly why your doctor and pharmacist need to know every single thing you take, including over-the-counter medicines and even herbal supplements. Total transparency is your best safety tool.
How Your Body's Health Plays a Role
It's not just other substances that matter; your own body's condition is a huge factor. Your liver and kidneys are the main players when it comes to processing flecainide and clearing it from your system.
If you have liver or kidney disease, these organs might work a bit slower. This means flecainide could build up to higher-than-expected levels, raising the risk of the serious side effects flecainide can cause. It's like a sink drain that isn't clearing water as fast as it should.
Your doctor's decision on your flecainide dose is a highly personalized calculation. They consider your age, how well your kidneys and liver are working, and your overall health to find that sweet spot between effectiveness and safety.
This is why you'll have regular blood tests to check on your organ function. It's a standard part of being on this medication and allows your doctor to make sure your dose is still the right one for you over time.
Being upfront about everything, from a new supplement you're thinking of trying to any changes in your health, gives your doctor the full picture. This partnership is what keeps your treatment working well and, most importantly, keeps you safe.
Being an Active Partner in Your Heart Health
When you're managing your heart health on flecainide, it's a team sport, and you're the most valuable player. This isn't just something happening to you; it's a journey you actively shape alongside your doctor. Taking a proactive role is the best way to make sure your treatment is both safe and successful.

This starts with understanding why your doctor schedules regular check-ins, blood tests, and ECGs. These aren't just boxes to tick. Think of them as vital safety checks. Each one provides a crucial piece of the puzzle, giving your doctor a clear picture of how your body is handling the medication and helping them spot any potential issues before they grow.
Why Ongoing Monitoring Is So Important
While you're on flecainide, your doctor is keeping a close eye on a few key things. Regular ECGs, for example, let them measure specific changes in your heart’s electrical signals, like the QRS interval. A little change is expected, but too much can be a warning sign.
Blood tests are just as critical. They help your doctor check how well your liver and kidneys are doing their jobs. Since these are the organs that process and clear flecainide from your body, making sure they're in good shape is essential to prevent the drug from building up to unsafe levels. This careful monitoring helps minimize the risk of serious side effects flecainide can cause.
Your regular appointments are your opportunity to be seen and heard. They are the cornerstone of a safe treatment plan, allowing for personalized adjustments based on your body's unique response to the medication.
Using Your At-Home ECG as a Powerful Tool
Many people now have at-home ECG devices, and they can be an incredible asset on this journey. The key is to use these tools not to self-diagnose, but to gather high-quality information to share with your medical team. You are the expert on how you feel day-to-day. When you combine that personal experience with objective data, it's powerful.
For instance, when you feel a symptom, a flutter, a moment of dizziness, taking an ECG reading right then provides invaluable context. It connects what you're feeling with what your heart is actually doing.
To make this information truly helpful for your doctor, here are a few tips:
- Document Everything: Keep a simple journal. Note the date, time, and what you were doing when a symptom popped up. Had you just exercised? Were you feeling stressed?
- Connect Symptoms to Readings: Next to your notes, jot down what the ECG showed during that episode. For example, "Felt fluttery after climbing stairs, ECG showed..."
- Look for Patterns: Over time, you might notice that certain activities or times of day seem to trigger your symptoms. This is incredibly useful information for your doctor.
Having More Productive Doctor Visits
Imagine walking into your appointment ready and organized. Instead of just saying, "I've been feeling a bit off," you can say, "Last Tuesday at 3 PM, I felt a strong palpitation, and here's the ECG from that moment."
This kind of clear, data-backed communication helps your doctor make the most informed decisions about your care. It turns you into a true collaborator in your health, building a stronger, more trusting partnership. By taking on this active role, you aren't just managing a medication; you're steering your own health journey with confidence.
Frequently Asked Questions About Flecainide
Starting a new medication can bring up a lot of questions. Getting good answers is a huge part of feeling in control of your health. Let's walk through some of the most common things people wonder about when they start taking flecainide.
How Long Do Flecainide Side Effects Last?
Many of the more common side effects, like feeling dizzy or having blurry vision, are usually most noticeable right after you start the medication. The good news is that for most people, these feelings ease up or go away completely within a few days to a couple of weeks as their body gets used to flecainide.
But if those effects feel intense or just aren't getting better, it's really important to let your doctor know. Whatever you do, don't just stop taking flecainide on your own. That can be dangerous.
Can I Drink Alcohol While Taking Flecainide?
This is a great question, and it's one you absolutely need to discuss with your doctor, because the answer is different for everyone. Alcohol can make side effects like dizziness worse. For some people, alcohol can even be a direct trigger for their atrial fibrillation.
Your doctor knows your whole health picture and how you're responding to the medication, so they can give you advice that's specific to you. The safest bet is always to follow their guidance.
The rule of thumb for a missed dose is simple: take it as soon as you remember. But if it's almost time for your next dose, just skip the one you missed and get back on your regular schedule.
What If I Miss a Dose of Flecainide?
It's really important not to double up on your next dose to make up for a missed one. Taking too much at once increases your risk of side effects.
A great tip is to ask your pharmacist for their specific instructions on this when you first pick up your prescription. That way, you'll know exactly what the plan is if it happens.
Qaly provides expert-reviewed analyses of your smartwatch ECGs, helping you track symptoms and understand what’s happening with your heart’s rhythm.










.png)
.png)