Key Takeaways
Heart failure is a chronic, progressive condition in which the heart muscle is unable to pump enough blood to meet the body’s needs for blood and oxygen. It doesn’t mean the heart has stopped working, but rather that it’s not working as efficiently as it should. Living with heart failure can be challenging, but understanding the condition and how to manage it can significantly improve quality of life.
What Causes Heart Failure?
Heart failure typically develops because of other conditions that have damaged or weakened the heart. Common causes include:
- Coronary Artery Disease (CAD): The most common cause, where narrowed arteries reduce blood flow to the heart muscle, weakening it over time.
- High Blood Pressure (Hypertension): Uncontrolled high blood pressure forces the heart to work harder, leading to thickening and stiffening of the heart muscle.
- Heart Attack: A heart attack can damage a portion of the heart muscle, impairing its pumping ability.
- Diabetes: Chronic high blood sugar can damage blood vessels and nerves, and directly affect the heart muscle.
- Valvular Heart Disease: Damaged or diseased heart valves can force the heart to work harder to pump blood.
- Cardiomyopathy: Diseases of the heart muscle itself, which can be genetic, caused by infections, alcohol abuse, or other factors.
Types of Heart Failure
Heart failure can affect either the left side, right side, or both sides of the heart.
- Left-sided heart failure is the most common type and occurs when the left ventricle can’t pump enough blood to the body. This can lead to fluid buildup in the lungs (pulmonary edema).
- Right-sided heart failure occurs when the right ventricle can’t pump enough blood to the lungs, leading to fluid buildup in the legs, ankles, and abdomen.
ECGs and Heart Failure
An ECG (electrocardiogram) is a standard tool used in the diagnosis and management of heart failure. While it cannot definitively diagnose heart failure on its own (an echocardiogram is typically needed for that), it can provide valuable clues about the underlying causes and the extent of heart damage.
What You Might See on a 1-Lead ECG in Heart Failure
While a 1-lead ECG (like those from smartwatches or portable devices) doesn’t provide a complete view of heart function, it can still reveal important rhythm-related clues. Here are some findings that may be visible:
- Appears as an irregularly irregular rhythm with no distinct P waves.
- Very common in heart failure and can worsen symptoms.
- Often reliably detected on a single-lead ECG.

2. Ventricular Tachycardia (VT) or Ventricular Fibrillation (VF)
- May show as wide, fast, or chaotic QRS patterns.
- These are serious arrhythmias and medical emergencies. A 1-lead ECG may capture them if recorded during an episode.
_apple.webp)
- QRS complexes that appear smaller than usual in amplitude.
- Can suggest fluid buildup around the heart (pericardial effusion), which is sometimes seen in advanced heart failure.

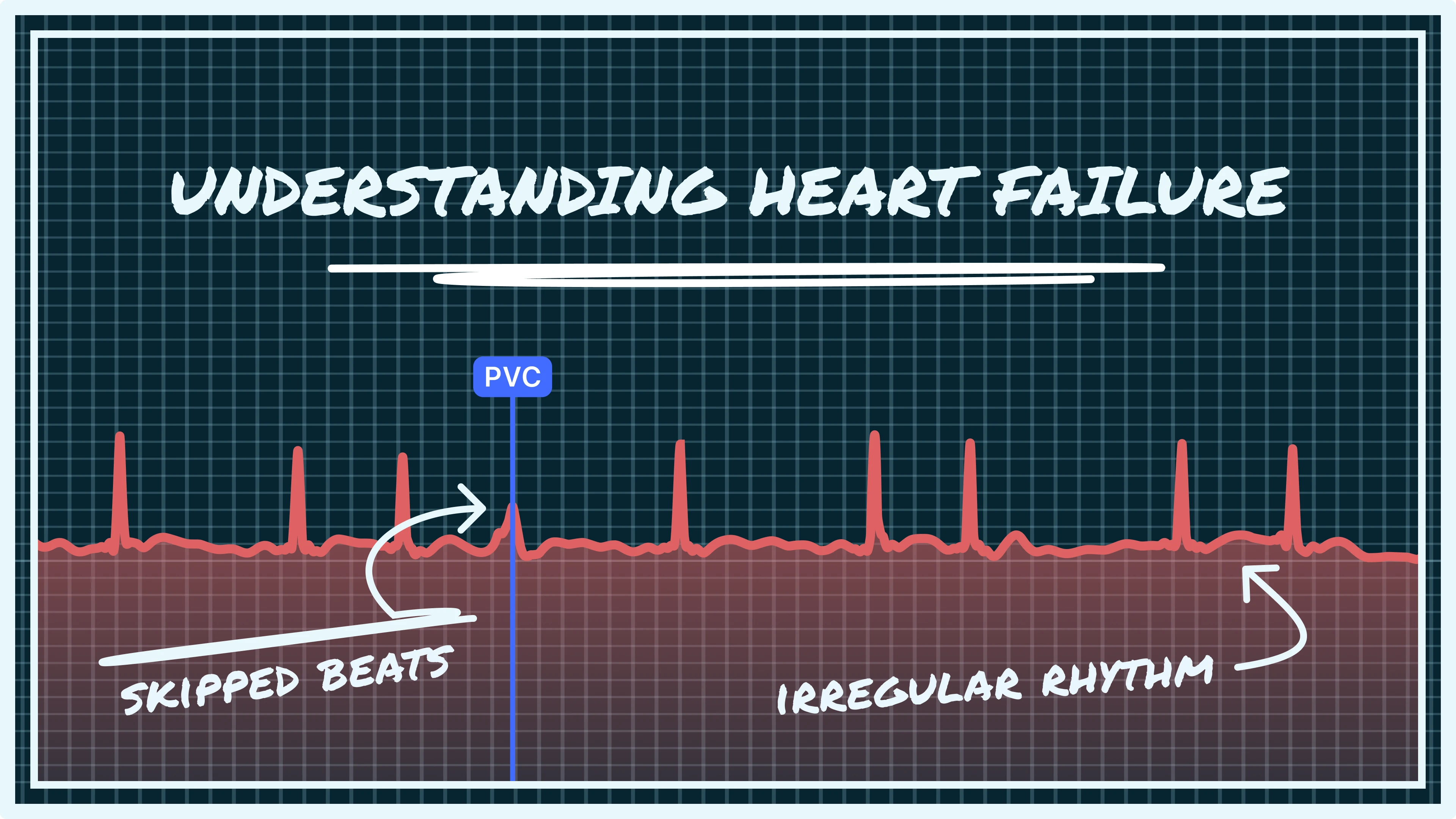
4. Irregular Heart Rhythms or Ectopic Beats
- Your device may detect extra beats, skipped beats, or irregular timing, which can be signs of underlying arrhythmias common in heart failure.
.webp)
Note: Many important heart failure-related ECG findings — including Left Ventricular Hypertrophy (LVH), bundle branch blocks, pathological Q waves (from prior heart attacks), and ST-T wave changes — are typically not reliably visible on a 1-lead ECG. A full 12-lead ECG is required to assess these patterns accurately. Any irregular findings on a 1-lead device should be followed up with your healthcare provider.
Symptoms of Heart Failure
The symptoms of heart failure often develop gradually and can worsen over time. They are primarily due to the heart’s inability to pump enough blood to meet the body’s demands, and fluid buildup.
Common Symptoms of Heart Failure:
- Shortness of Breath (Dyspnea): Especially during exertion or when lying flat (orthopnea), often relieved by sitting up or using extra pillows.
- Fatigue and Weakness: Due to reduced blood flow to muscles and organs.
- Swelling (Edema): In the legs, ankles, feet, and sometimes the abdomen, due to fluid retention.
- Rapid or Irregular Heartbeat: Palpitations or a feeling that your heart is racing.
- Persistent Cough or Wheezing: With white or pink blood-tinged mucus, due to fluid in the lungs.
- Reduced Exercise Capacity: Difficulty performing activities that were once easy.
- Increased Urination at Night: As fluid shifts when lying down.
- Lack of Appetite and Nausea: Due to fluid buildup around the digestive system.
Managing Heart Failure
Managing heart failure involves a comprehensive approach aimed at improving symptoms, preventing progression, and enhancing quality of life.
Lifestyle Modifications
- Dietary Changes: Limiting sodium intake is crucial to reduce fluid retention.
- Regular Exercise: Moderate physical activity can improve symptoms and overall quality of life.
- Weight Management: Maintaining a healthy weight reduces the heart’s workload.
- Quit Smoking and Limit Alcohol: Both can worsen heart failure.
- Monitor Symptoms and Weight Daily: Track changes and alert your doctor to sudden weight gain or symptom changes.
Medications
Several classes of medications are used to treat heart failure:
- ACE Inhibitors or ARBs: Relax blood vessels and reduce the heart’s workload.
- Beta-Blockers: Slow heart rate and reduce blood pressure.
- Diuretics: Help the body eliminate excess fluid.
- Mineralocorticoid Receptor Antagonists (MRAs): Improve heart function.
- SGLT2 Inhibitors: Diabetes medications that also benefit heart failure patients.
- ARNI (Angiotensin Receptor-Neprilysin Inhibitor): A newer combination drug with strong benefits in heart failure.
Devices and Procedures
For some individuals, advanced therapies may be necessary:
- Implantable Cardioverter-Defibrillator (ICD): Reduces risk of sudden cardiac death.
- Cardiac Resynchronization Therapy (CRT): Helps the heart beat more efficiently in cases with conduction delays.
- Heart Transplant or Ventricular Assist Devices (VADs): Options for end-stage heart failure.
Conclusion
Understanding heart failure and how it may appear on your ECG is an important step in managing your condition. While a 1-lead ECG from your smartwatch or portable device cannot show everything, it can still provide valuable insight into your heart’s rhythm, especially when it comes to detecting irregularities like atrial fibrillation, skipped beats, or fast rhythms.
If you are living with heart failure, being aware of these changes and monitoring your ECG regularly can help you stay ahead of potential issues. However, a 1-lead ECG is only one part of the overall picture. It should always be interpreted alongside your symptoms, lab results, physical exams, and imaging such as an echocardiogram.
At Qaly, we are here to help you understand your heart data. Our team of experts can review your smartwatch ECGs and help you make sense of what you are seeing, so you can feel more informed, more confident, and more in control of your heart health. To get started, simply download the Qaly app from the App Store or get it on Google Play.
Stay proactive, stay connected, and as always from the team at Qaly, stay heart healthy ❤️
Watching for heart failure rhythm changes? Qaly experts review your smartwatch ECGs in minutes. Start monitoring today.









.png)
.png)