Key Takeaways
That unsettling flutter or sudden fainting spell can be alarming, especially when it comes without warning. These experiences might be linked to a condition known as Long QT Syndrome (LQTS), a heart rhythm disorder that, while often hidden, can have serious implications. This guide aims to shed light on LQTS, helping you understand its complexities and what it means for your heart health.
Deciphering the Electrical Glitch: What is Long QT Syndrome?
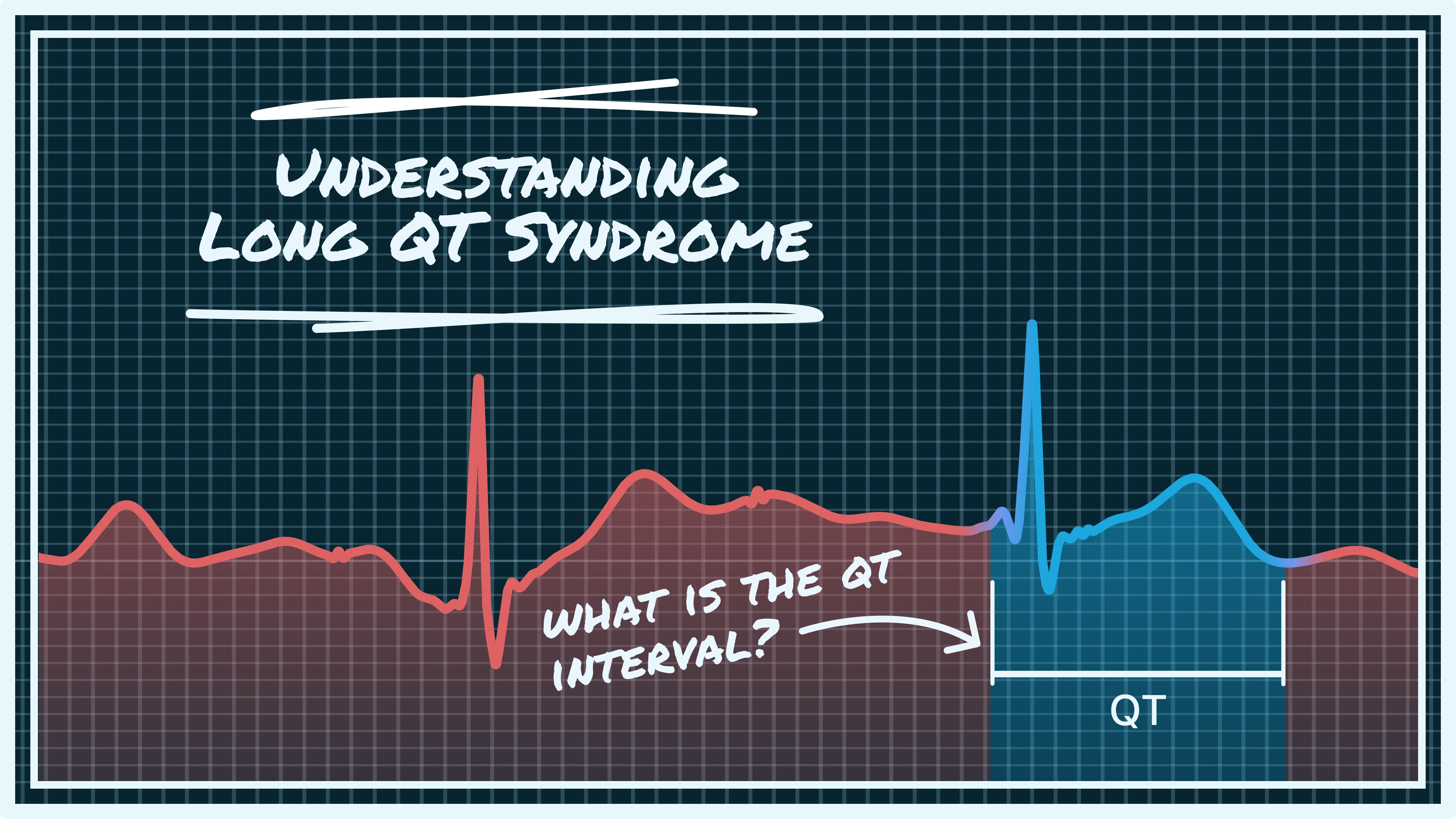
Your heart is an extraordinary organ, tirelessly pumping blood throughout your body, a feat orchestrated by a precise electrical system. Each heartbeat is a carefully choreographed dance of electrical signals that cause your heart muscle to contract and relax. This electrical activity is captured and visualized on an electrocardiogram (ECG), where different waves and intervals represent specific phases of your heart's cycle.
One crucial segment on the ECG is the QT interval. It represents the time it takes for your heart's ventricles (the lower pumping chambers) to contract and then fully recharge for the next beat. Think of it like a battery: after expending its energy to power a contraction, it needs a moment to fully recharge before it can fire again. In Long QT Syndrome, this recharging process takes longer than it should, leading to an abnormally prolonged QT interval.

This delay in recharging makes the heart vulnerable to chaotic and life-threatening arrhythmias, particularly a rapid, irregular heartbeat called Torsades de Pointes. While the heart's physical structure may be perfectly normal, the electrical instability caused by a prolonged QT interval can lead to sudden, dangerous heart rhythms.
The Roots of LQTS: What Causes a Prolonged QT Interval?
Long QT Syndrome isn't a one-size-fits-all condition; its origins can be broadly categorized into two main types: inherited (congenital) and acquired.
Inherited Long QT Syndrome
In most cases, LQTS is a genetic condition, passed down through families. It's caused by mutations in specific genes that are responsible for creating and regulating the ion channels in your heart cells. These ion channels—primarily potassium, sodium, and calcium channels—control the flow of electrical currents in and out of the heart cells, which is vital for the heart's normal rhythm. When these channels don't function correctly due to a genetic mutation, the heart's recharging process is disrupted, leading to a prolonged QT interval.
Several types of inherited LQTS exist, each linked to different gene mutations. For instance, LQT1, LQT2, and LQT3 are the most common forms, associated with mutations in potassium and sodium channel genes. If a family member has been diagnosed with LQTS, or if there's a history of unexplained sudden death in the family, genetic testing may be recommended to identify the specific mutation.
Acquired Long QT Syndrome
Unlike the inherited form, acquired LQTS develops later in life and is not due to genetic mutations. It's often a side effect of certain medications or an imbalance in the body's chemistry. A wide range of drugs can prolong the QT interval, including:
- Antiarrhythmic drugs: Medications used to treat other heart rhythm disorders, such as sotalol and amiodarone.
- Antibiotics: Certain types, like macrolides (e.g., azithromycin) and fluoroquinolones (e.g., ciprofloxacin).
- Antihistamines: Some non-sedating antihistamines.
- Antidepressants and antipsychotics: Various medications used for mental health conditions.
- Antifungals: Certain antifungal agents.
Beyond medications, electrolyte imbalances play a significant role in acquired LQTS. Low levels of potassium (hypokalemia), magnesium (hypomagnesemia), or calcium (hypocalcemia) can all interfere with the heart's electrical stability and prolong the QT interval. Other contributing factors can include severe bradycardia (very slow heart rate), hypothyroidism, hypothermia, and certain underlying heart conditions.
Understanding the cause of LQTS is crucial for effective management and treatment, as the approach will differ significantly between inherited and acquired forms. Always inform your healthcare provider about all medications you are taking and any family history of heart conditions.
The Silent Signals: Recognizing the Symptoms of Long QT Syndrome
One of the most challenging aspects of Long QT Syndrome is that many individuals with the condition experience no symptoms at all. LQTS might only be discovered incidentally during a routine ECG or after a significant cardiac event. However, for those who do experience symptoms, they can range from mild and infrequent to severe and life-threatening. These symptoms often occur when the heart rate increases, such as during physical exertion, emotional stress, or even during sleep.
The most common and often the first symptom of LQTS is fainting, also known as syncope. These fainting spells can occur suddenly and without warning, often triggered by intense emotions (like anger or surprise), loud noises, or strenuous exercise. The fainting happens because the prolonged QT interval leads to a dangerous arrhythmia, causing a temporary reduction in blood flow to the brain. In some cases, these fainting spells can be mistaken for seizures.
Other symptoms that may indicate LQTS include:
- Palpitations: A sensation of a fluttering, pounding, or racing heart in the chest.
- Dizziness or lightheadedness: A feeling of being unsteady or about to faint.
- Gasping during sleep: This can be a particularly concerning symptom, as it may indicate a nocturnal cardiac event.
- Seizure-like activity: While not true seizures, the lack of oxygen to the brain during an arrhythmia can mimic seizure symptoms.
- Sudden cardiac arrest: In the most severe cases, LQTS can lead to sudden cardiac arrest, where the heart abruptly stops beating effectively. This can be fatal if not immediately treated.
- Near-drowning or drowning incidents: In children, unexplained drowning or near-drowning incidents can sometimes be the first sign of LQTS, as the stress of swimming can trigger an arrhythmia.
It's important to note that these symptoms are not exclusive to LQTS and can be caused by many other conditions. However, if you experience any of these symptoms, especially if they are recurrent or occur during triggers like exercise or emotional stress, it is crucial to seek medical attention promptly. A thorough evaluation by a healthcare professional can help determine the underlying cause and ensure appropriate management.
Unveiling the Unseen: Diagnosing Long QT Syndrome
Diagnosing Long QT Syndrome can be complex, particularly because symptoms may be absent or mimic other conditions. The diagnostic process typically involves a combination of medical history, physical examination, and specialized cardiac tests. The primary tool for diagnosing LQTS is the electrocardiogram (ECG).
The Electrocardiogram (ECG)
An ECG is a non-invasive test that records the electrical activity of your heart, and even a single-lead ECG can provide valuable insights. In the case of Long QT Syndrome (LQTS), the focus is on measuring the QT interval. While a standard 12-lead ECG is traditionally used, one-lead ECGs like those captured by smartwatches or personal ECG devices can still be useful, especially when recorded regularly. Since the QT interval can fluctuate and be influenced by factors like stress, sleep, and medications, capturing multiple ECGs over time (even with a single lead) can help detect abnormal patterns.
Beyond the Standard ECG: Additional Diagnostic Tools
To gain a more comprehensive understanding of your heart's electrical activity and to confirm a diagnosis of LQTS, your doctor may recommend additional tests:
- Holter Monitor: This portable ECG device is worn for 24 to 48 hours, or sometimes even longer (up to several weeks), to continuously record your heart's rhythm during your daily activities. This can help capture intermittent QT prolongation or arrhythmias that might not be present during a brief in-office ECG.
- Exercise Stress Test: During this test, you walk on a treadmill or ride a stationary bike while your heart rate and ECG are monitored. Exercise can sometimes unmask QT prolongation or arrhythmias that are not apparent at rest.
- Genetic Testing: Since many cases of LQTS are inherited, genetic testing can be crucial for confirming a diagnosis, identifying the specific gene mutation, and screening family members. This can help in risk stratification and guiding treatment decisions.
- Blood Tests: These tests are performed to check for electrolyte imbalances (such as low potassium, magnesium, or calcium) and to assess thyroid function, as these can cause acquired forms of LQTS.
- Echocardiogram: An ultrasound of the heart, an echocardiogram provides images of your heart's structure and function. While LQTS is primarily an electrical disorder, this test can help rule out other structural heart problems.
Diagnostic Criteria and Scoring Systems
Given the variability in LQTS presentation and the potential for overlapping symptoms with other conditions, clinicians often rely on established diagnostic criteria and scoring systems to aid in accurate diagnosis. The most widely used is the Schwartz Score, a clinical diagnostic tool that assigns points based on various factors, including ECG findings, clinical history, and family history. A higher score indicates a greater probability of LQTS.
Key components of the Schwartz Score include:
- ECG Findings: This is the most heavily weighted component, with points awarded for significant QTc prolongation (e.g., QTc ≥ 480 ms), Torsades de Pointes (a specific type of dangerous arrhythmia), and T-wave alternans (subtle beat-to-beat variations in T-wave morphology).
- Clinical History: Points are given for unexplained syncope (fainting) or seizures, especially if triggered by exercise, emotion, or auditory stimuli.
- Family History: A history of LQTS in first-degree relatives or unexplained sudden death in young family members significantly increases the score.
While a Schwartz Score of 3.5 or higher is generally considered diagnostic for LQTS, and a score between 1.5 and 3 indicates intermediate probability, it's important to remember that this is a clinical tool and not a definitive test on its own. It guides clinicians in determining the likelihood of LQTS and the need for further investigation, such as genetic testing.
Early and accurate diagnosis of Long QT Syndrome is vital. It allows for the implementation of appropriate management strategies, which can significantly reduce the risk of life-threatening cardiac events and improve the quality of life for individuals with the condition. If LQTS is suspected, a referral to a cardiologist or an electrophysiologist (a heart rhythm specialist) is often recommended for expert evaluation and personalized care.
Conclusion
That wraps up our guide on Long QT Syndrome and the importance of understanding your QT interval. We hope it gave you clarity on what the QT interval is, why it matters, and how to recognize when it might be too long.
We know that monitoring your QT interval can feel overwhelming. That’s exactly why we built the Qaly app. Whether you’re tracking your QT over time or trying to make sense of a single concerning result, our human ECG experts can help. On Qaly, we’ll review your QT and QTc intervals within minutes, so you’re not left wondering or waiting.
To get started, download the Qaly app from the App Store or Play Store today. And if you have any questions or need further support, feel free to reach out to us anytime at support@qaly.co.
Have trouble measuring your QTc Interval? On the Qaly app, human experts will measure your ECGs' QTc Interval within minutes. Get started today.









.png)
.png)