Key Takeaways
Hello Heart Hero. Feeling your heart flutter, pound, or skip a beat can be unsettling. It’s completely normal to feel a little worried when it happens.
Most of the time, heart palpitations are just harmless blips caused by everyday things like stress, caffeine, or a tough workout. But sometimes, they can be a sign of an underlying heart rhythm issue, which is why it’s so important to understand what might be triggering them.
Your Guide to Understanding Heart Palpitations
Feeling your own heartbeat can be a strange, sometimes frightening experience. One moment, everything is fine, and the next, you're suddenly aware of a flutter, a thud, or a racing sensation in your chest. If you've felt this, you're not alone. And you're certainly not alone in wanting clear, trustworthy answers, especially when the healthcare system can feel confusing or impersonal.
What Exactly Is a Heart Palpitation?
Simply put, a heart palpitation is the sensation of being aware of your own heartbeat. It’s not a specific medical condition, but a symptom that can feel different for everyone. For some, it's a brief flutter. For others, it’s a sustained, hard pounding that you can feel in your neck or throat.
Think of your heart as a skilled drummer, usually keeping a steady, quiet beat you don't even notice. A palpitation is like a moment when that drummer suddenly breaks the rhythm, hitting a loud, unexpected beat or a rapid-fire sequence that grabs your full attention. It’s that sudden, surprising awareness that defines the experience.
Most of the time, this little "drum solo" is temporary and totally harmless, but its unpredictability is what can be so unnerving. Understanding what might cause these palpitations is the first step toward figuring out if it's a benign hiccup or something that needs a closer look.
A key thing to remember is that palpitations are a symptom, not a diagnosis. They are a signal from your body, and our job is to learn how to interpret that signal without unnecessary fear.
Why You're Seeking Answers
It's all too common to feel dismissed when you bring up symptoms like palpitations. Maybe you've been told "it's just stress" without getting a clear path forward. This guide is different. It respects your concerns and recognizes that you’re taking a proactive role in your health.
We’ll explore the many different reasons for these sensations, from everyday triggers to specific heart rhythm changes. We'll cover topics like:
- How emotional states like anxiety can directly impact your heart's rhythm.
- Common lifestyle triggers such as caffeine, alcohol, and even certain medications.
- Underlying heart rhythm changes and what they actually mean in simple terms.
We’ll start with a quick overview of the most common causes, giving you a simple framework before we dive deeper into each one. This way, you’ll feel empowered and informed every step of the way on your journey to better heart health.
How Stress and Anxiety Can Trigger Palpitations
It might surprise you to learn that for many people, the root cause of heart palpitations isn't some dangerous heart condition. Instead, it’s the powerful connection between your mind and your body.
Feeling that sudden flutter or pounding in your chest when you're stressed or anxious is a very real, very physical response. Understanding this link is the first step toward regaining a sense of control.
When you experience stress, your body can't tell the difference between a looming work deadline and an actual tiger chasing you. It reacts the same way it has for thousands of years: by kicking on the "fight or flight" response. This is your body’s built-in survival system.
This system floods your body with hormones like adrenaline, which basically acts like a gas pedal for your heart. It tells your heart to beat faster and harder to pump more blood to your muscles, getting you ready to either face the danger or run from it. This sudden surge is what you feel as a racing heart or a forceful pounding in your chest.

Why Anxiety Feels So Physical
Anxiety is more than just a feeling of worry; it's a state of high alert that keeps your fight or flight system simmering on low. Even chronic, low-level stress can keep adrenaline circulating, making your heart extra sensitive to sudden changes in rhythm.
This can create a really frustrating cycle. You feel anxious, which triggers a palpitation. The palpitation itself feels scary, which then ramps up your anxiety, leading to even more palpitations. Breaking this loop starts with recognizing that the sensation, while alarming, is often just a normal reaction to your emotional state.
Curious about the specifics? We dive deeper into this topic in our detailed article on how anxiety can cause heart palpitations.
The link is well-documented. In a study of 190 adults with palpitations, anxiety or panic disorders were the cause in 31% of cases, making it the second most common reason right after actual cardiac issues. The World Health Organization also points out that with more than 1 in 8 people worldwide living with an anxiety disorder, palpitations are a key physical complaint for a huge number of people.
Taming the Adrenaline Rush
Realizing that your emotions can directly influence your heartbeat is actually quite empowering. It means you have the power to influence it, too. When you feel that familiar flutter starting, think of it as a signal from your body to check in with how you're feeling emotionally.
Here are a few ways stress can physically show up as palpitations:
- Sudden Scares: A loud noise or a near-miss in traffic can cause a jolt of adrenaline, resulting in a brief, forceful heartbeat.
- Chronic Worry: Ongoing stress from work, finances, or relationships can keep your nervous system on high alert, leading to more frequent flutters or a constantly elevated heart rate.
- Panic Attacks: During a panic attack, the body gets an intense surge of the fight or flight response, often causing a rapid, pounding heart that can last for several minutes.
Remember, a palpitation caused by anxiety is not a sign of heart weakness. It’s a sign of your body's strength and its natural, protective instinct to keep you safe from what it perceives as a threat.
Learning to manage the sources of stress is key to reducing these episodes. Simple techniques like deep breathing, mindfulness, and gentle exercise can help calm your nervous system and slow your heart rate.
When Your Heart's Rhythm Is the Underlying Cause
While stress and anxiety are huge triggers for heart palpitations, sometimes that fluttering sensation is a sign of a genuine change in your heart's electrical rhythm. This is called an arrhythmia, and while the word sounds intimidating, it simply means your heart's beat has gone off-kilter.
Thinking about your heart's electrical system can feel complicated, but let's break it down. Imagine your heart has its own internal pacemaker, sending out signals to keep a steady beat, almost like a drummer in a band. An arrhythmia happens when this drummer misses a beat, adds an extra one, or suddenly starts playing way too fast.
The goal here isn't to diagnose you, that's what your doctor is for. Instead, my aim is to demystify these terms so you can have more confident conversations with your healthcare provider and better understand what your personal ECG device might be showing you.
Common Types of Arrhythmias
Not all rhythm changes are the same. Some are incredibly common and often harmless, while others need a closer look. Let's walk through a few of the most frequent types you might come across.
Premature Ventricular Contractions (PVCs)
A PVC is one of the most common reasons people feel a "skipped beat." Think of it as an extra, early beat that fires off from the heart's bottom chambers (the ventricles). Because it happens too soon, it disrupts the normal rhythm, often followed by a brief pause and then a stronger, more noticeable beat as the heart gets back on track.
This can feel like:
- A flip-flop or flutter in your chest.
- A hard thud that seems to come out of nowhere.
- The distinct sensation of a skipped beat.
For most people, occasional PVCs are completely benign and can be brought on by things like caffeine, stress, or a poor night's sleep.
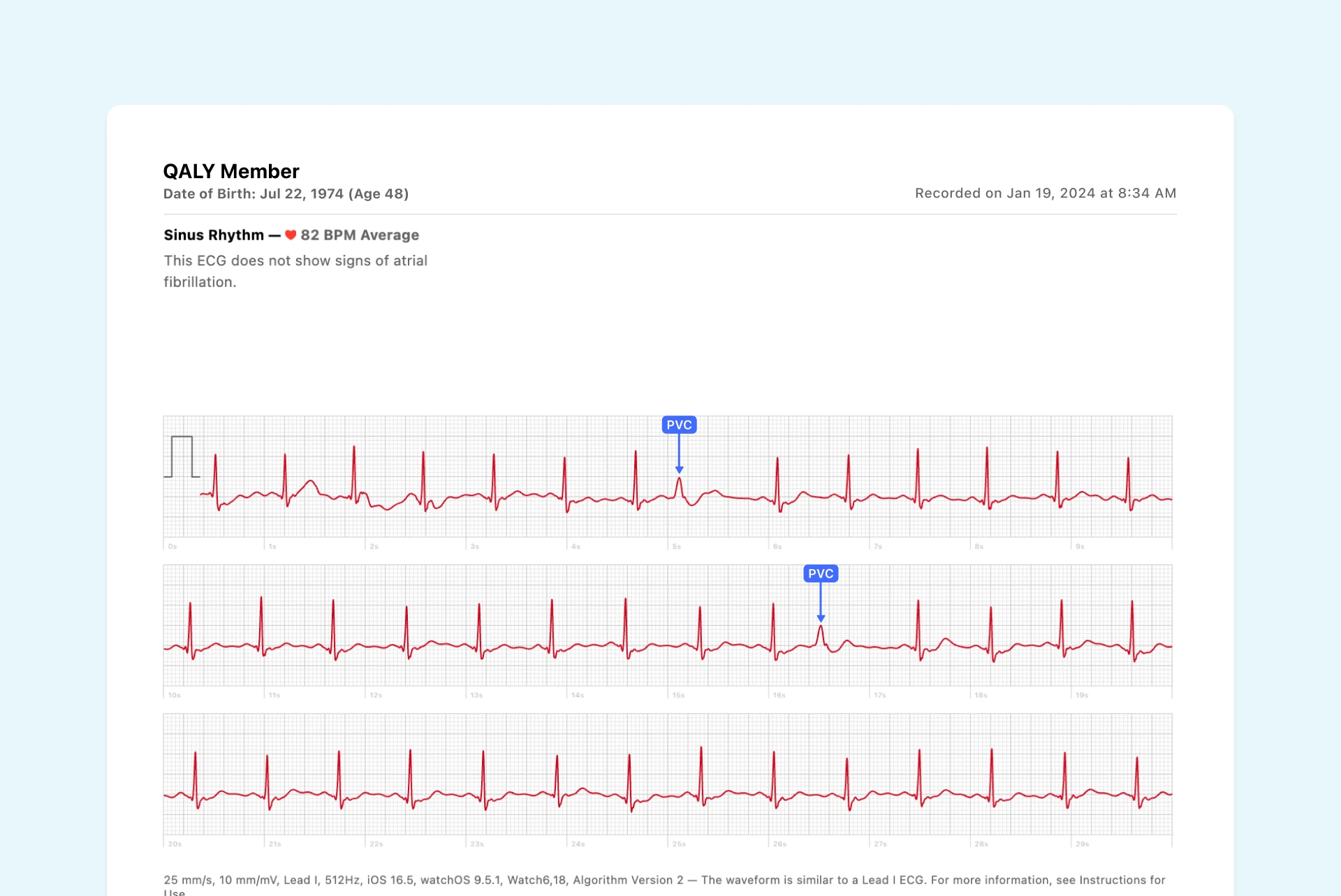
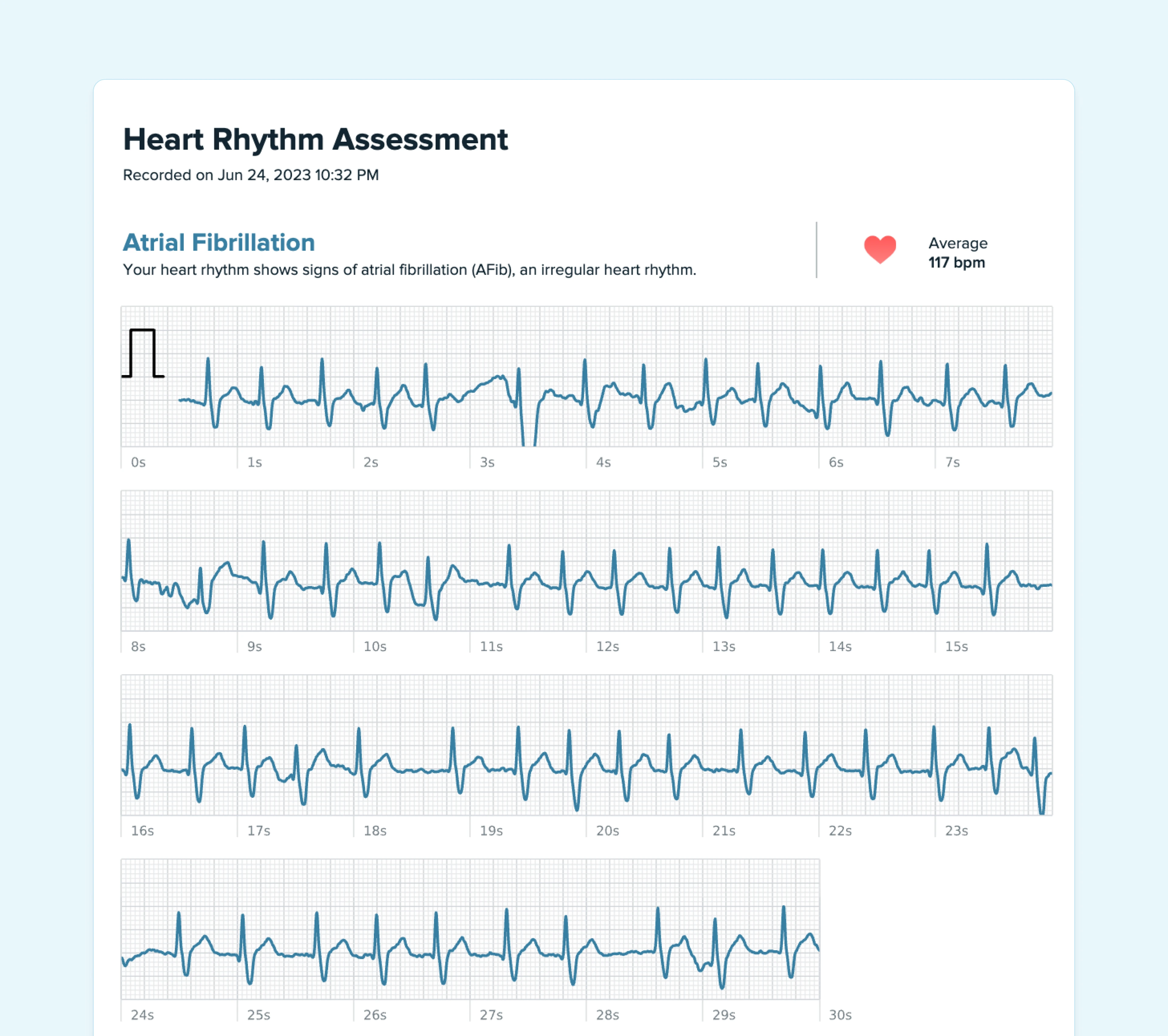
Atrial Fibrillation (AFib)
AFib is a totally different beast. Instead of just one extra beat, the heart's top chambers (the atria) start to quiver chaotically. This sends rapid, disorganized signals down to the bottom chambers.
Sticking with our drummer analogy, AFib is like the drummer suddenly abandoning the steady beat and just rattling the drums randomly and unpredictably. This creates a rhythm that doctors often describe as "irregularly irregular."
This can feel like a sustained fluttering, a racing heart, or a completely disorganized quivering sensation that might last for minutes or even hours.
Putting It All in Context
It's completely normal to feel anxious when you hear these medical terms. But knowledge is a powerful tool for dialing down that fear. Recognizing what these sensations might be is the first step toward getting clarity.
While anxiety is a major trigger, underlying rhythm changes are the single largest category of identified causes for palpitations. One comprehensive review of 190 patients found that 43% of palpitations were due to a cardiac cause. The most common culprits were premature beats (like PVCs), supraventricular tachycardia (SVT), and atrial fibrillation (AFib).
-2-example.webp)
These events are often missed during a quick doctor's visit because they come and go, which is why capturing the rhythm yourself during an episode is so important. If you want to dive deeper, you can explore the findings of this palpitations research here.
Understanding the basics of what a heart rhythm disorder is can provide even more context and peace of mind. Check out our guide explaining what is a heart rhythm disorder for a clearer picture. Ultimately, having this information helps you work with your doctor as a more informed partner in your own health.
Identifying Lifestyle Triggers for Heart Flutters
Sometimes, the answer to "what's causing my heart palpitations" isn't a complex medical issue, but something hiding in your daily routine. It’s incredibly empowering to realize just how much your habits, diet, and even natural life stages can influence your heart’s rhythm. This is where you get to be a detective for your own health, spotting potential triggers you can actually control.
Think of your heart as a sensitive instrument. Just like a guitar string can vibrate from a loud noise nearby, your heart can react to certain substances or hormonal shifts in your body. Let’s look at some of the most common culprits that might be behind those surprising flutters.
The Jolt from Stimulants
Many of us lean on a little boost to get through the day, but these same stimulants can sometimes give your heart an unwelcome jolt. They work by exciting your central nervous system, which can ramp up your heart rate and make it more prone to an extra beat here and there.
The usual suspects include:
- Caffeine: That morning cup of coffee, tea, or energy drink is a classic. Caffeine can make some people's hearts race or skip a beat. Everyone’s sensitivity is different, so what’s fine for your friend might be too much for you.
- Nicotine: Found in cigarettes, vaping products, and other tobacco items, nicotine is a powerful stimulant. It directly impacts heart rate and blood pressure, often acting as a clear trigger for palpitations.
- Certain Medications: It’s not just about coffee and cigarettes. Some over-the-counter cold and cough medicines contain ingredients like pseudoephedrine, which is designed to shrink nasal passages but can also speed up your heart as a side effect.
If you’re a coffee lover, it helps to understand its specific effects. You can learn more by examining coffee's impact and whether it's good or bad for your heart in our detailed guide.
Paying attention to when your palpitations happen can give you huge clues. Do they show up after your second espresso? Or when you've taken a decongestant for a stuffy nose? Keeping a simple log can help you connect the dots.
How Alcohol and Dehydration Play a Role
While many people think of alcohol as a relaxant, it can be a significant trigger for heart palpitations. It has a knack for interfering with the heart's electrical signals. It can also lead to dehydration and electrolyte imbalances, all of which create the perfect environment for irregular heartbeats to pop up.
For sensitive people, even a single drink can be enough to set off an episode. This is sometimes called "holiday heart syndrome," a phenomenon where people experience arrhythmias after a bout of heavier drinking.
On top of that, simple dehydration on its own can be a cause. When you don't have enough fluids, your blood volume can decrease. This forces your heart to work harder to pump blood, and that extra strain can sometimes show up as palpitations.
Hormonal Shifts and Your Heartbeat
Your body’s hormones are powerful chemical messengers that regulate countless functions, including your heart rate and rhythm. So, when these hormone levels fluctuate, it’s not uncommon to feel it in your chest.
These natural shifts are a very common, though often overlooked, reason for palpitations, especially for women.
Key periods of hormonal change include:
- Menstruation: The rise and fall of estrogen and progesterone during the menstrual cycle can definitely influence heart rhythm.
- Pregnancy: During pregnancy, a woman's blood volume increases by up to 50%. This forces the heart to work harder and beat faster, which can lead to frequent palpitations.
- Menopause: The decline in estrogen during perimenopause and menopause is also associated with an increase in heart flutters and racing sensations.
Beyond these life stages, an overactive thyroid gland (hyperthyroidism) can be the culprit. This condition floods your body with too much thyroid hormone, which basically acts like a constant stimulant, speeding up both your metabolism and your heart rate.
Ultimately, these lifestyle and bodily factors are often things you can manage. Research shows that substances like caffeine and alcohol, along with hormonal changes, are frequently identified as triggers. For instance, in one study, about 6% of palpitations were directly linked to drugs or substances, highlighting just how much our daily choices can matter.
Using Wearable ECGs to Get Real Answers
Does this sound familiar? You’ve been feeling a strange flutter in your chest for days, but the second you walk into the doctor’s office, it’s gone. This maddening experience is why getting answers about heart palpitations can feel like a wild goose chase. You're not imagining it, and you're definitely not alone.
The heart of the problem is that palpitations are often fleeting. A standard ECG in a clinic only captures a few seconds of your heart’s activity. It’s like trying to photograph a hummingbird with a slow-shutter camera, you’re almost guaranteed to miss the action.
This is where at-home, wearable ECG devices are a total game-changer. These incredible tools, often built right into smartwatches or available as small handheld monitors, put the power to capture your heart’s rhythm directly into your hands. You no longer have to hope your symptoms show up on cue for a doctor’s appointment.
Capturing the Moment That Matters
Imagine feeling that familiar flutter, but instead of just worrying, you place your fingers on your watch and record your ECG in that exact moment. This ability to capture your heart's electrical activity during a symptom is a massive breakthrough. It transforms a fleeting, subjective feeling into concrete, objective data that you and your doctor can finally dig into.
The low success rate of traditional tests often comes down to timing. Standard 12-lead ECGs see less than a minute of your rhythm, and even 24-48 hour Holter monitors can completely miss infrequent events. This is changing fast, though. Consumer ECGs let you activate a recording the instant symptoms appear, dramatically boosting the odds of catching the culprit.
Turning Data into Understanding
Having the raw ECG data is a fantastic first step, but it’s only half the battle. Staring at a bunch of squiggly lines can feel confusing and might even create more anxiety if you don't know what you’re looking at. This is where modern services come in, bridging the gap between simply having information and actually understanding what it means for you.
Instead of waiting weeks for a specialist, you can have your ECG reviewed by a certified cardiographic technician in minutes. This gives you two incredibly valuable things:
- Immediate Reassurance: In many cases, the technician can confirm a rhythm is benign, like a common PVC, giving you instant peace of mind and breaking the anxiety cycle.
- Actionable Reports: If something more significant is detected, you get a clear, human-verified report you can confidently share with your doctor. Your next appointment shifts from a conversation about vague feelings to a productive discussion based on real evidence.
This process is all about moving from a state of passive worry to one of proactive health management. You become an active participant in your own care, armed with the information needed to have meaningful conversations with your healthcare team.
If you own a smartwatch with an ECG feature, knowing how to use it is a great place to start. We cover this in our cardiologist's guide to the smartwatch ECG, which can help you get the most out of your device.
Knowing When to Seek Immediate Medical Care
While most heart palpitations are just harmless flutters, it's vital to recognize the signals that point to a more urgent problem. This isn't meant to scare you; it’s here to empower you. Knowing the difference between a benign flutter and a serious warning sign helps you respond the right way, getting care when you need it and avoiding unnecessary worry.
Think of it like this: a single, isolated palpitation is like your body sending a simple notification. But a palpitation paired with other serious symptoms? That’s your body sending a high-priority alert with a blaring siren. These are the alerts you absolutely need to pay attention to.
Understanding the Red Flags
Certain symptoms are critical warning signs. They suggest the palpitation might be from an arrhythmia that's preventing your heart from pumping blood effectively.
According to guidelines from major health organizations, palpitations that come with fainting (syncope), feeling like you’re about to faint, chest pain, or severe shortness of breath demand immediate attention. Another crucial factor is a family history of sudden cardiac death at a young age, which should always prompt a thorough evaluation. You can learn more about these urgent symptoms and their causes from trusted medical sources.
If you experience a palpitation along with any of the following symptoms, it’s time to seek immediate medical care. Don’t wait it out or second-guess yourself.
Here are the key red flags to watch for:
- Severe Dizziness or Lightheadedness: A strong sensation that you might pass out.
- Fainting (Syncope): Actually losing consciousness, even just for a moment.
- Significant Shortness of Breath: Trouble breathing that feels unusual or severe for you.
- Chest Pain or Pressure: Any kind of discomfort, tightness, or pain in your chest.
Ultimately, you have to trust your body. If a palpitation feels intensely different and shows up with these other symptoms, getting it checked out right away is the safest and most proactive step you can take.
Common Questions About Heart Palpitations
When you start paying attention to your heart, it’s only natural to have a few questions pop up. Feeling a flutter or a skipped beat can be unnerving, and getting straight answers is the first step to feeling back in control. Let's tackle some of the most common concerns we hear every day.
Our goal here is to cut through the confusion and give you clear, practical information. Think of this as a conversation to replace that nagging uncertainty with solid knowledge, so you can better understand what your body is telling you.
Can Heart Palpitations Be a Sign of a Heart Attack?
This is the big one, the question that’s often at the front of everyone's mind. So let’s get right to it. While a change in heartbeat can happen during a heart attack, palpitations by themselves are not a classic sign.
A heart attack typically comes with a whole different set of much more dramatic symptoms. These are the real red flags.
The key is to look at the bigger picture. A palpitation becomes a serious concern when it shows up with these classic heart attack warnings:
- Chest Pain or Pressure: This isn’t just a little ache. It’s a feeling of tightness, squeezing, or heavy pressure in the chest that might radiate to your arms, back, neck, or jaw.
- Severe Shortness of Breath: A sudden, overwhelming struggle to catch your breath.
- Breaking Out in a Cold Sweat: Unexpected, profuse sweating for no apparent reason.
- Extreme Weakness or Nausea: A sudden, crushing feeling of sickness or fatigue that floors you.
If you experience palpitations alongside any of these other symptoms, that’s your signal to seek emergency medical care immediately.
How Long Can Harmless Palpitations Last?
This varies a ton from person to person. For most people, a harmless palpitation is a blink-and-you-miss-it event, a single "thump" or a quick flutter that’s over in a second or two. These are incredibly common and usually nothing to worry about.
Sometimes, it might feel more like a short burst of rapid beats, lasting for several seconds. Even these are often perfectly benign, especially if you can connect them to an obvious trigger, like a sudden jolt of adrenaline, a strong cup of coffee, or a wave of anxiety.
A good rule of thumb is that the context matters more than the duration. A few seconds of fluttering after your morning espresso is one thing. But if you have a sustained, rapid heartbeat that makes you feel dizzy or unwell for 30 seconds or more, that’s a different story and definitely warrants a call to your doctor.
Can Heart Palpitations Go Away on Their Own?
Yes, absolutely. In fact, many of them do. When palpitations are tied to lifestyle factors or emotional stress, they often fade away once the trigger is gone or the stress is managed. For instance, if you realize your flutters are caffeine-driven, simply cutting back can make them vanish.
It's the same for anxiety-related palpitations; as you practice stress-reducing techniques like deep breathing or mindfulness, you may notice them happen less and less. Even harmless arrhythmias like occasional PVCs can be intermittent, with long stretches where you don't feel them at all. This is exactly why figuring out your personal triggers is one of the most powerful things you can do.
Navigating palpitations can feel isolating, but you don't have to do it alone. With Qaly, you can get your wearable ECG reviewed by a certified expert in minutes, any time of day.










.png)
.png)