Key Takeaways
Hello, Heart Hero. Seeing the words "abnormal ECG T wave" on a report can feel instantly jarring. It’s a technical term that sounds serious, and it’s easy to feel anxious or lost, especially if you're feeling unheard by the traditional healthcare system. This guide is here to be your calm, clear translator and empower you with knowledge.
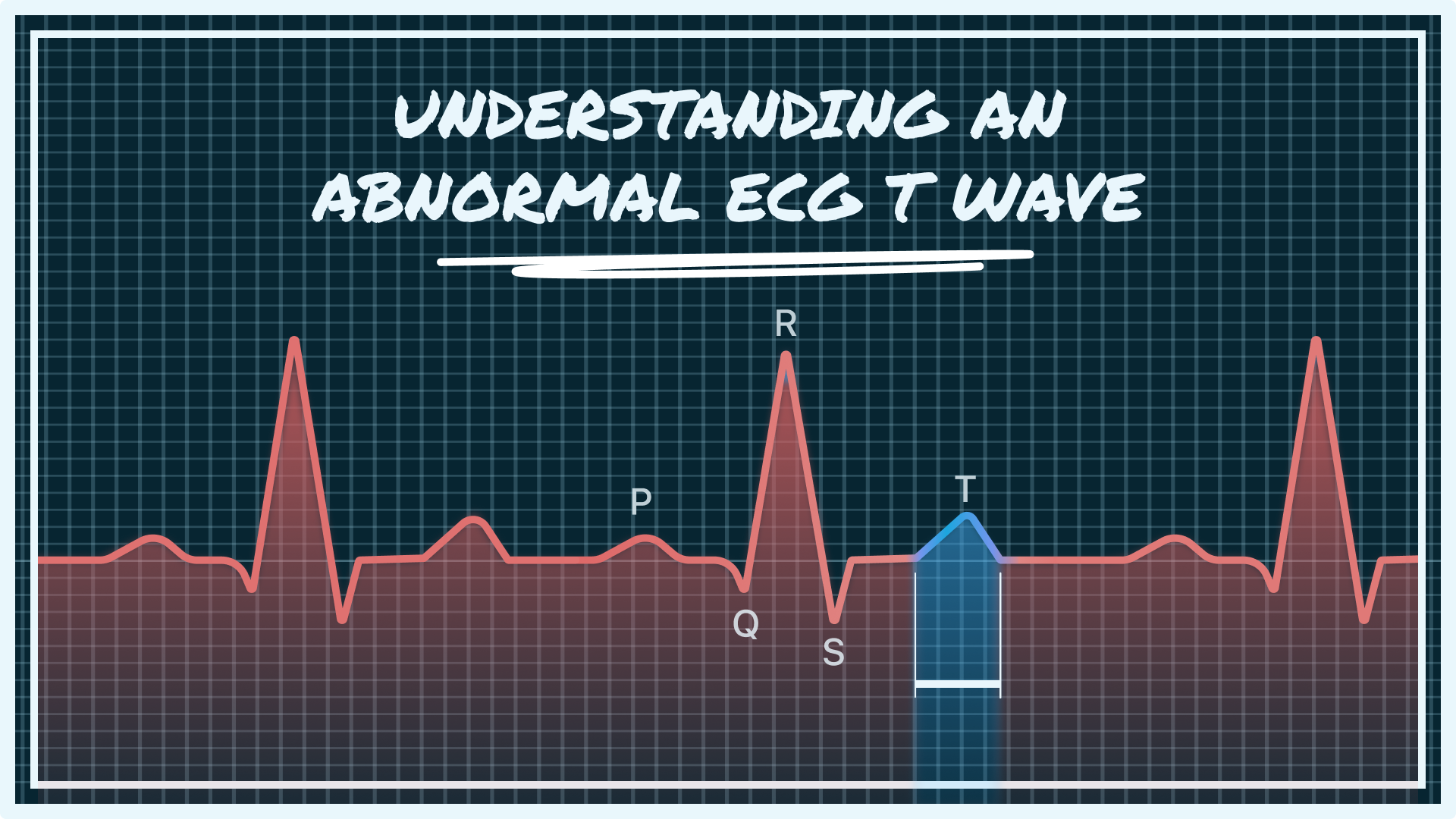
An abnormal ECG T wave is a change in the final part of your heart's electrical signal. This part of the ECG represents the heart muscle "recharging" between beats. While it can be a sign of a heart condition, it often has many other, less serious causes. A single reading isn't a diagnosis - it's a signal to investigate further.
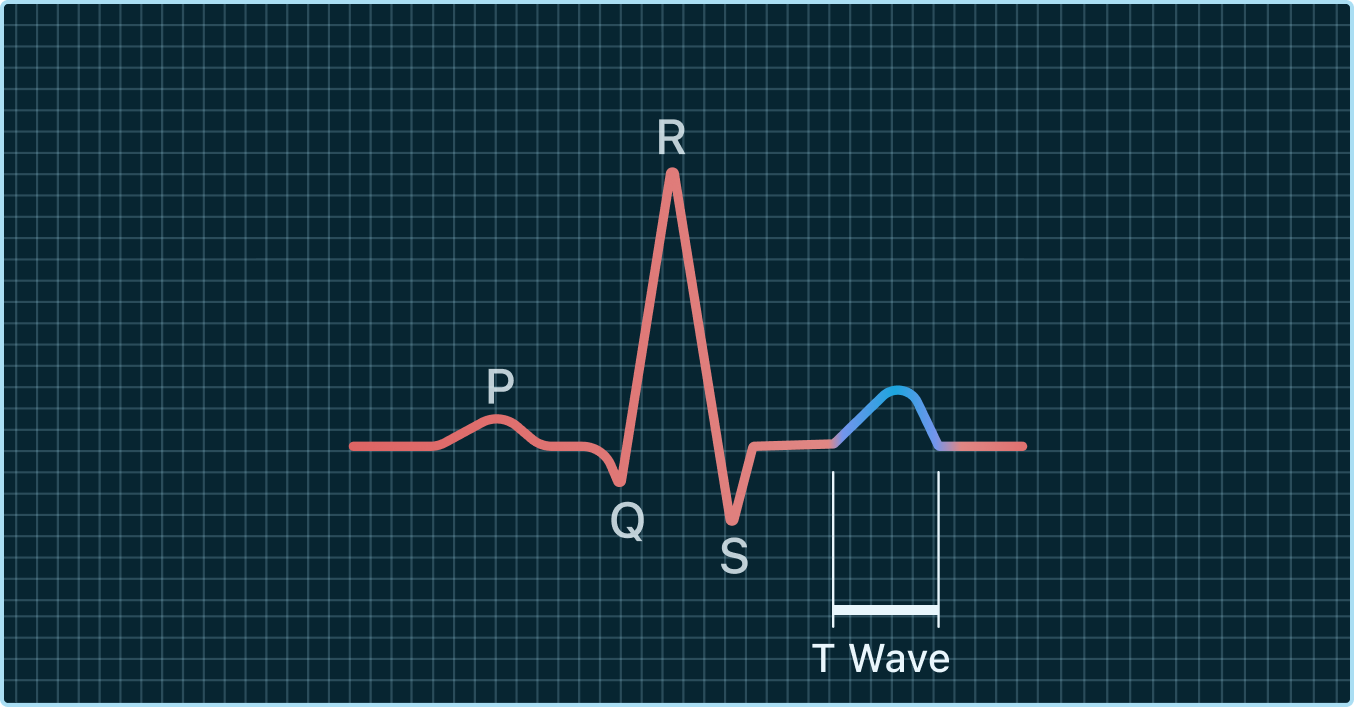
Your Guide to the ECG T Wave
Think of your heart's electrical rhythm as a short piece of music that repeats with every beat. Each part of the ECG tells a story about what your heart is doing at that moment. The T wave is simply the final note, showing that your heart's main pumping chambers (the ventricles) are resting and resetting for the next beat.
Demystifying the "Abnormal" Label
An "abnormal" T wave is just a signal, not an immediate verdict. It simply means the shape, size, or direction of this "recharging" wave is different from what's considered typical. But "different" doesn't always mean dangerous.
Many things can influence your T wave, and it's crucial to understand that context is everything. Your doctor's job is to be a detective, using this clue to look at the bigger picture of your health. An isolated abnormal T wave without any other symptoms often just leads to a simple follow-up, not an emergency. You can learn more about the broader context in our guide to understanding the general abnormal ECG meaning.
Why This Signal Matters to You
This part of your ECG gets attention because it provides a window into your heart's electrical stability and the overall health of its muscle. A consistent, well-formed T wave suggests the recharging process is happening smoothly. A change might indicate that something is affecting that process.
Here’s why understanding this matters for your peace of mind:
- It’s a Clue, Not a Conclusion: It prompts a closer look, which is a good thing. It's an opportunity for proactive care.
- Many Causes Are Benign: Things like stress, a hard workout, or even electrolyte levels from dehydration can cause temporary changes.
- Knowledge is Power: Understanding what it means allows you to have a more confident and informed conversation with your doctor, ensuring your concerns are heard and addressed.
Our goal is to replace confusion with clarity. By understanding your heart's unique rhythm, you can move from a place of worry to a position of empowerment, ready to partner with your healthcare team effectively.
This guide will walk you through what the T wave represents, what different shapes can mean, and what the common causes are, giving you the tools you need to feel in control of your heart health journey.
What a T Wave Reveals About Your Heartbeat
Let's demystify the T wave together. Imagine your heart is a high-tech battery that powers your entire body. With every single beat, it sends out a powerful electrical surge to pump blood. On an ECG, this powerful surge is that tall, sharp spike you see - the QRS complex. But just like any battery, your heart needs to recharge after each use.
The T wave is the visual signal of that recharging process. In medical terms, this is called ventricular repolarization, which is just a fancy way of saying your heart's main pumping chambers are resetting themselves for the next beat.
The Analogy of a Camera Flash
Think about an old-school camera with a flash. You press the button, and FLASH, a huge burst of energy lights up the room. That's like your heart's powerful contraction, the QRS complex.
But then, you have to wait a moment. You might even hear a faint, high-pitched whine as the flash recharges its capacitor, getting ready for the next picture.
The T wave is that gentle recharging whine. It's a quieter, slower, and equally crucial part of the cycle. A healthy, upright T wave shows that this reset is happening smoothly and efficiently. It's the sign of a well-oiled machine, ready for action.
A normal T wave is the heart's quiet promise that it has successfully reset and is prepared for the next beat. It signifies electrical stability and readiness.
Why Doctors Pay Close Attention to the T Wave
So, why is this "recharging" wave so important? The shape, size, and direction of the T wave give doctors valuable clues about the health of your heart muscle.
This reset phase is incredibly sensitive to what's happening inside your body. It can be affected by:
- Oxygen Levels: If your heart tissue isn't getting enough oxygen-rich blood, the recharging process can be disrupted, which changes the T wave's shape.
- Electrolyte Balance: Minerals like potassium and calcium are essential for your heart's electrical wiring. An imbalance can directly impact repolarization and show up as an abnormal ECG T wave.
- Structural Health: The physical condition of the heart muscle itself plays a huge role in its ability to reset properly after each beat.
Think of it like a muscle relaxing after you’ve tensed it. If you clench your fist tightly and then let go, your hand returns to a relaxed state. The T wave is the electrical version of that relaxation. If the muscle is tired, strained, or not getting enough nutrients, it might not relax as smoothly - and this would be reflected in the T wave.
Because this phase is so sensitive, an abnormal T wave often acts as an early warning signal. It doesn't automatically mean something is seriously wrong, but it's a clear sign for your doctor to say, "Hey, let's take a closer look here." It’s a clue, not a conclusion.
A Visual Guide to Different T Wave Shapes
Not all "abnormal" T waves look the same, and getting to know the different variations is a powerful first step toward feeling more in control. Think of this as a simple field guide to the most common patterns you might see on an ECG report.
We’ll break down what these shapes can mean - not for self-diagnosis, but to give you the vocabulary to understand your heart’s story and have more informed conversations with your doctor.
An abnormal ECG T wave is simply one that deviates from that standard gentle, upright hill shape. But what do those deviations look like? They usually fall into a few key categories, and each one tells a slightly different tale about your heart's recharging process.
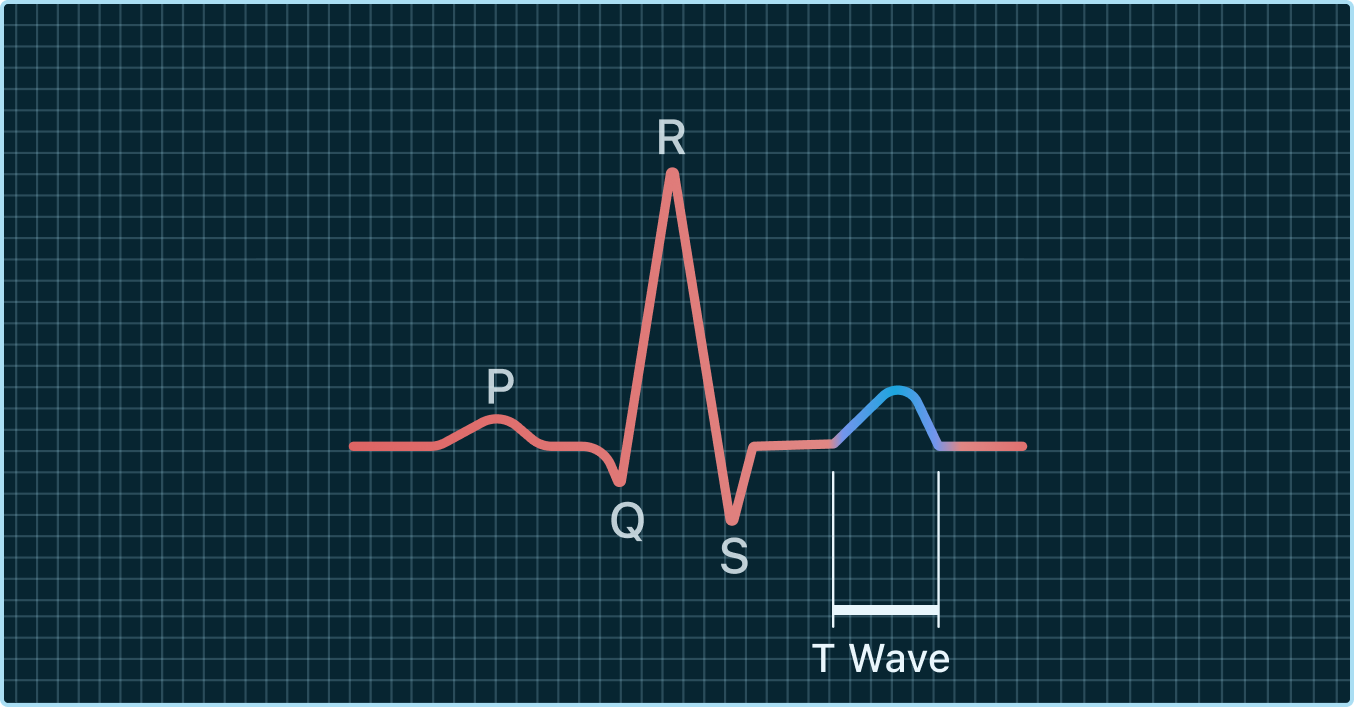
T Wave Inversion: When the Wave is Upside Down
One of the most frequent findings is T wave inversion. Instead of curving up after the main QRS spike, the T wave dips down, creating a valley where there should be a hill.
Seeing an inverted T wave can feel jarring, but context is everything. For some people, this can be a completely normal, lifelong finding on certain parts of their ECG. It doesn't automatically mean something is wrong.
In other situations, however, a newly inverted T wave can be a sign that part of the heart muscle isn't getting enough oxygen-rich blood - a condition called myocardial ischemia. This is precisely why a doctor will always compare a new ECG to any you've had in the past. It’s all about spotting changes.
Research backs this up. A long-term Finnish study of over 6,300 people found that T wave inversions in specific areas of the heart were linked to a higher risk of coronary heart disease. These findings show how doctors use the location of the inversion as a vital clue.
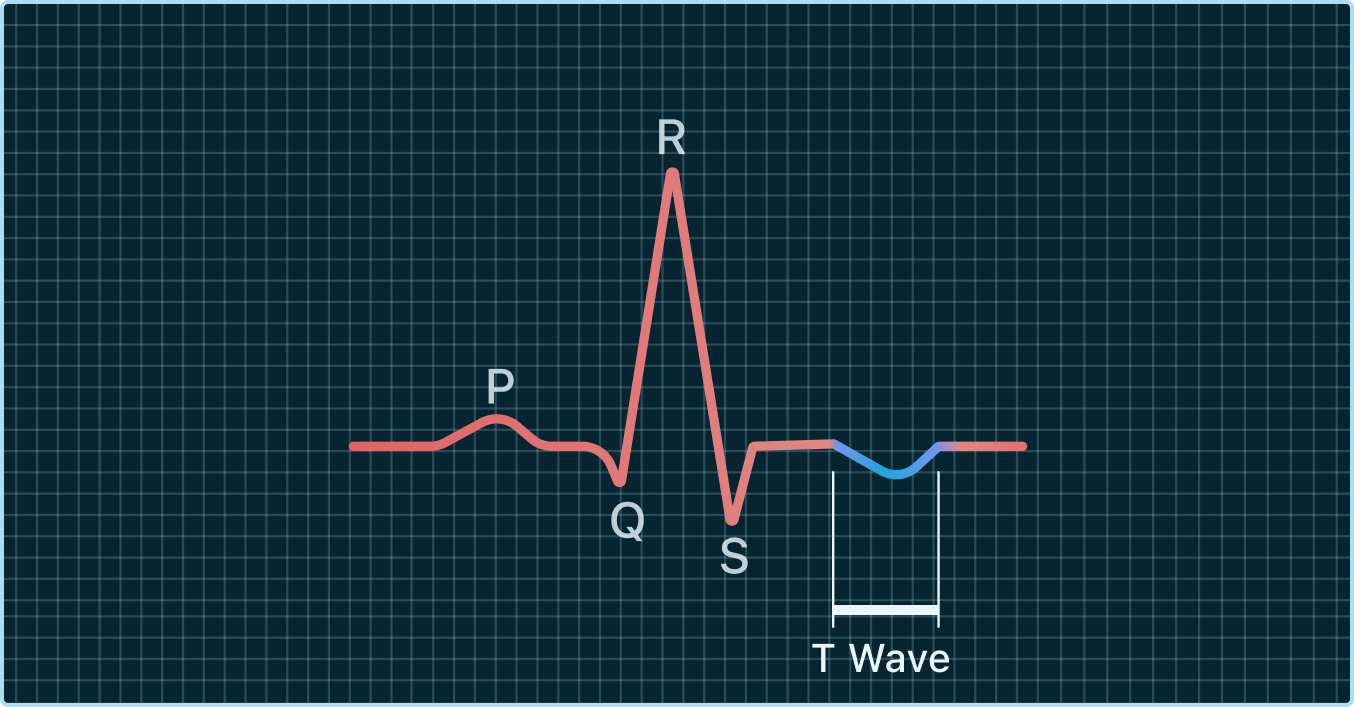
Flattened T Waves: A Barely-There Bump
Sometimes, the T wave isn’t upside down, but it’s much shorter or flatter than it should be. A flattened T wave looks like the gentle hill has been worn down into a small, low bump.

This is often connected to imbalances in your body's electrolytes, especially low potassium levels (hypokalemia). Potassium is a key player in the heart's electrical symphony, so when there isn't enough, the recharging signal gets weaker, causing the T wave to flatten. Dehydration, certain medications like diuretics, or some medical conditions can all lead to low potassium.
A flattened T wave is often a clue about a systemic issue, like an electrolyte imbalance, rather than a primary problem with the heart muscle itself. It’s a signal that your body's internal environment might need a little rebalancing.
Peaked T Waves: Tall and Pointed
The opposite of a flattened wave is a peaked T wave, sometimes called a hyperacute T wave. This is when the T wave is unusually tall, narrow, and pointed - looking more like a tent than a gentle hill.
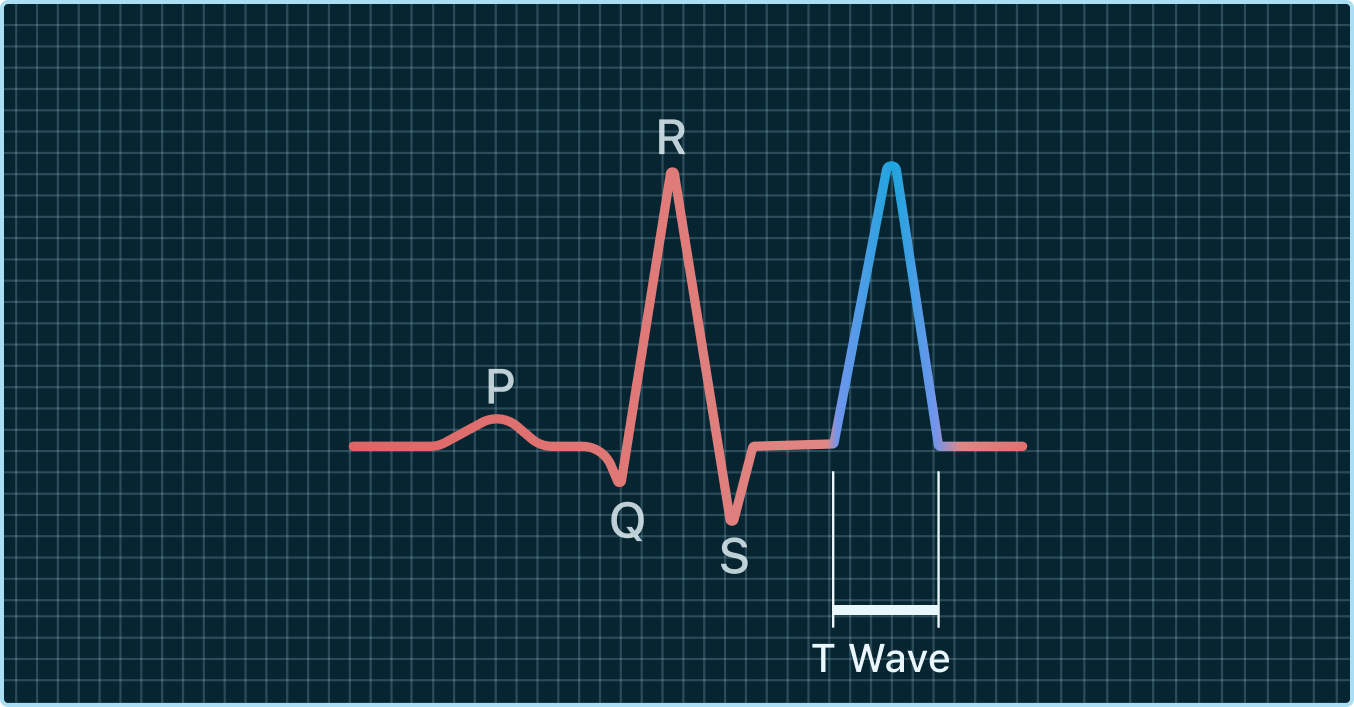
This is a classic sign of high potassium levels (hyperkalemia). Just as too little potassium weakens the signal, too much can make it overly strong and sharp. High potassium is a serious condition that requires prompt medical attention because it can disrupt the heart's rhythm.
Separately, in the very early stages of a heart attack, peaked T waves can sometimes be the first warning sign on an ECG, appearing even before other, more obvious changes. It’s a pattern doctors take very seriously for this reason.
Common T Wave Abnormalities at a Glance
This table breaks down the different T wave shapes and their common potential meanings in a simple, visual way. Remember, a doctor must interpret these findings in the context of your overall health.
By familiarizing yourself with these shapes, you're better equipped to understand the language of your ECG. It helps turn a potentially confusing report into something you can discuss with your healthcare team, making you an active partner in your own health journey.
Exploring the Common Causes of T Wave Changes
It’s completely natural to feel a jolt of worry when you see a note about an “abnormal T wave.” Our minds often jump to the most serious conclusions. But before you go down that rabbit hole, take a deep breath. An abnormal T wave is simply a clue, and it can point to a wide range of factors - many of which are not related to a serious heart condition at all.
This section is here to give you a balanced look at what might be behind the change. Think of your doctor as a detective. The T wave is the first clue they find, and their job is to piece together the full story. Let's look at the list of "usual suspects" they consider, from heart-related issues to everyday lifestyle influences.
Heart-Related Clues Your Doctor May Investigate
When a T wave looks different, your healthcare provider will first consider conditions directly tied to the heart. These are often the first things to rule out just to make sure your heart is working as it should.
Here are a few common cardiac causes:
- Myocardial Ischemia: This is the medical way of saying "reduced blood flow to the heart muscle." When heart cells don't get enough oxygen, it affects how they "recharge" after a beat (a process called repolarization), which can cause T waves to flip upside down.
- Pericarditis: This is when the thin sac surrounding your heart, the pericardium, gets inflamed. This irritation can interfere with the heart's electrical signals and lead to widespread changes across the ECG, including the T waves.
- Cardiomyopathy: This term covers diseases of the heart muscle itself, like an enlarged or thickened heart. When the heart's physical structure changes, its electrical properties often change, too, which can show up as an abnormal ECG T wave.
- Past Heart Attack: Sometimes, a previous heart attack may have gone unnoticed. The scar tissue it leaves behind can cause persistent T wave abnormalities in specific areas of an ECG.
It's important to remember that these are just possibilities your doctor will explore. An abnormal T wave does not automatically mean you have one of these conditions. It's simply a starting point for a thoughtful investigation.
The Powerful Influence of Electrolytes
Your heart’s electrical system is incredibly sensitive to the balance of minerals in your blood, known as electrolytes. Even tiny shifts can create very noticeable changes on an ECG.
The most common culprits here are potassium and magnesium. For example, low potassium levels (hypokalemia), which might happen from dehydration, certain medications like diuretics, or even severe vomiting, can cause T waves to flatten out. On the flip side, very high potassium (hyperkalemia) can make T waves tall and pointy.
This connection is so strong that doctors often check electrolyte levels as one of the first steps after seeing a T wave change. To learn more about this, check out our guide on how an electrolyte imbalance and your ECG are closely linked.
Non-Cardiac Causes You Might Not Expect
This is where things get really interesting, and often, quite reassuring. Many T wave changes are triggered by things that have nothing at all to do with heart disease. This is a crucial part of the puzzle that sometimes gets overlooked, leaving people to worry for no reason.
Here are some of the most common non-cardiac influences:
- Intense Exercise: A really tough workout can temporarily alter your heart's electrical activity. This sometimes causes T wave inversions that disappear once you've recovered, and it's especially common in endurance athletes.
- Stress and Anxiety: High levels of stress hormones like adrenaline can directly impact your heart's rhythm and electrical signals. This can lead to temporary T wave changes that are completely benign.
- Certain Medications: A whole host of medications can affect the heart's recharging phase. This includes some antidepressants, antipsychotics, and even certain antibiotics.
- Neurological Events: Conditions affecting the brain, like a stroke or a severe head injury, can sometimes cause dramatic changes on an ECG, including deep T wave inversions.
Understanding this wide spectrum of possibilities helps show why an abnormal T wave is just a clue for your doctor, not a final verdict. It’s the beginning of a conversation and a deeper look into your unique health, empowering you to be part of the solution.
What an Abnormal T Wave Means for Your Health
Hearing that your T wave is “abnormal” can definitely bring up a lot of questions. What does this really mean for you and your health? It's easy to feel a little anxious, especially when you’re trying to make sense of medical terms in a healthcare system that can feel pretty impersonal.
But let’s reframe this. An abnormal ECG T wave isn't a diagnosis in itself. Instead, doctors see it as a risk marker. Think of it as an early flag, a signal that lets your medical team be proactive instead of reactive. It's a chance to get a clearer picture of your heart health before a small issue becomes a bigger one.
An Early Warning System for Your Heart
This little signal on your ECG is often the starting point for a deeper conversation. It's not the end of the story. Your doctor might suggest more specific tests to understand what's really going on, like blood work to check electrolytes, an echocardiogram to see your heart's structure, or a stress test to watch how your heart handles pressure.
This proactive approach is a good thing. It gives you and your doctor a valuable opportunity to make positive changes, whether that means simple lifestyle adjustments, a new medication, or just a plan for closer monitoring. The goal is to use this early information to your advantage and take control.
Understanding the Clinical Significance
While many T wave abnormalities are harmless, it's important to understand why they're taken seriously. Changes in the T wave can be the very first sign of underlying issues that might affect your heart down the road.
For instance, T wave abnormalities on an ECG are recognized as significant predictors of sudden cardiac death (SCD), which is responsible for about 50% of all cardiovascular deaths globally. Research has shown that even minor changes can be linked to a higher risk of SCD and lower survival rates in adults. If you want to dive deeper, you can learn more about the research on T wave abnormalities as risk predictors.
Think of an abnormal T wave like a "check engine" light in your car. It doesn't mean the engine has failed - it just means it's time to have a professional look under the hood to see what's going on and prevent a breakdown.
From Diagnosis to Empowerment
The real power here is in what you do with this information. An abnormal ECG T wave gives you a head start. It's a sign that empowers you to ask smarter questions, advocate for your own health, and become an active partner with your doctor.
It helps you focus on real, actionable steps:
- Lifestyle Changes: You can get serious about improving your diet, getting more active, or managing stress, all of which directly impact your heart.
- Medication Adherence: If your doctor prescribes medication, you'll have a better understanding of why it's so important for keeping your heart stable.
- Closer Monitoring: You can keep a better eye on any symptoms and report changes quickly, which helps prevent potential complications from sneaking up on you.
Ultimately, this signal isn't a judgment. It's a guide for the road ahead. It’s an invitation to understand your body better and take proactive steps to protect your heart, especially if you're managing other conditions like heart failure. You can learn more by checking out our guide on understanding heart failure and what it looks like on your ECG.
Your Next Steps and When to Seek Advice
If you've just seen an abnormal ECG T wave on a report from your doctor, it's completely normal to feel a bit of uncertainty. The medical terms can be confusing, and it's easy to jump to conclusions.
The most important first step isn't to panic, but to plan a calm, informed conversation with your doctor. Think of this finding as a single clue, not a final diagnosis. A single ECG is just one snapshot in time, and it needs context. Your doctor’s job is to put this piece of the puzzle together with everything else they know about you.
When to Seek Immediate Medical Attention
While a simple follow-up is usually the right approach, certain symptoms should never be ignored. If you experience any of the following along with your ECG finding, it's time to get immediate medical care.
These are red flags that need a prompt evaluation:
- Chest Pain or Discomfort: Any new or unexplained pressure, squeezing, or pain in your chest.
- New or Worsening Shortness of Breath: Feeling like you can't catch your breath during normal activities or even at rest.
- Dizziness or Lightheadedness: A sudden feeling that you might pass out or that the room is spinning.
- Fainting (Syncope): Any time you lose consciousness.
- New, Strong Palpitations: A sudden feeling that your heart is racing, pounding, or skipping beats that feels different or more intense than usual.
These symptoms don't automatically mean something is seriously wrong, but they are your body's way of saying, "Pay attention now." It’s always better to get checked out and find out it’s nothing than to ignore a potentially serious signal.
Preparing for Your Doctor's Visit
Feeling prepared can turn that anxiety into action, helping you have a much more productive chat with your doctor. Being an active participant in your own care is powerful, especially when you’re trying to understand what’s going on.
Try to come to your appointment with a few things ready:
- A List of Your Symptoms: Jot down what you've been feeling, how often it happens, and what you were doing when it started.
- Your Medication List: This includes all prescriptions, over-the-counter drugs, and any supplements you're taking.
- Key Questions to Ask: Don't be shy about asking for clarity. Think about questions like, "What do you think is causing this change?" or "What are our next steps for figuring this out?"
This simple prep work helps you partner with your doctor to get the clear answers and care plan you deserve.
Frequently Asked Questions About T Waves
We get it. Seeing the words "abnormal T wave" on an ECG report can be unsettling and naturally brings up a lot of questions. Let's walk through some of the most common ones we hear to give you more clarity and, hopefully, some peace of mind.
First, remember that you're not alone in this. An abnormal ECG T wave is actually a pretty common finding. One major population-based ECG study of over 20,000 people found that minor T wave abnormalities showed up in about 20.4% of them, making it one of the most frequent observations.
Can Anxiety or Stress Cause an Abnormal T Wave?
Yes, absolutely. High levels of stress and anxiety can directly impact your body’s autonomic nervous system - the system that controls your "fight or flight" response. A surge of stress hormones like adrenaline can cause temporary, harmless changes to your ECG, including T wave abnormalities. It's one of the first non-cardiac causes doctors often consider.
Is an Inverted T Wave Always a Sign of a Heart Attack?
No, not at all. This is a very common fear, but it's often misplaced. While an inverted T wave can be a sign of reduced blood flow (ischemia) that might be related to a heart attack, it has many other potential causes.
For many people, an inverted T wave is just their normal, a harmless variation they've had their whole life. It can also be triggered by heart inflammation, electrolyte imbalances, and various other conditions. That's why the context of your symptoms, medical history, and the rest of your ECG is so critical for a proper interpretation.
Will an Abnormal T Wave Ever Go Back to Normal?
It's certainly possible. Whether a T wave abnormality can resolve depends entirely on its underlying cause. If the change is from something temporary or treatable (like an electrolyte imbalance from dehydration, a certain medication, or even high stress) your T wave may return to normal once that issue is addressed.
Your doctor's job is to play detective and figure out the "why" behind the signal. From there, they'll create a plan to manage the root cause, which can often lead to the T wave normalizing over time.
When you're dealing with the uncertainty of an abnormal ECG, the waiting game can be the hardest part. Qaly was created to close that gap, connecting you with certified experts who can interpret your smartwatch ECGs in minutes, day or night. Instead of spiraling into worry, get the clarity and peace of mind you deserve by having a professional review your heart's rhythm whenever you need it. Learn more and try Qaly for yourself at https://www.qaly.co.
Qaly’s experts can review your smartwatch ECGs (T wave interpretation coming soon!) to help you understand your heart. Start today









.png)
.png)