Key Takeaways
Hello Heart Hero. If you’ve ever felt that sudden, unnerving thump-thump in your chest and wondered what on earth is happening, take a deep breath. That menopause heart pounding sensation is an incredibly common experience during perimenopause and menopause, and it's most often tied to your fluctuating hormones, not a serious heart problem. It’s a very real physiological response to the changes your body is going through.
You are absolutely not alone in this. That feeling of your heart suddenly racing, fluttering, or pounding out of your chest can be deeply unsettling, especially when it comes out of the blue. We get it. Navigating these new symptoms can be frustrating, particularly when the healthcare system can sometimes feel dismissive or unhelpful. This guide is here to change that.
Our goal is to walk you through this with real empathy and clear information. We’ll explore the 'why' behind these sensations and arm you with the knowledge you need to feel more in control. By understanding what’s happening in your body, you can become your own best health advocate.

Understanding Menopause and a Pounding Heart
It’s a deeply unsettling feeling. Your heart suddenly starts pounding out of your chest for no reason, even when you're just trying to relax. The first step toward feeling less anxious and more in control is understanding why this is happening. The main culprit behind menopause-related heart pounding is the dramatic shift in your body's hormones.
Think of your hormones, especially estrogen, as a skilled conductor leading your heart's orchestra. For decades, estrogen has helped keep your heart's rhythm steady and smooth. It plays a huge role in keeping your blood vessels flexible and influencing your heart's entire electrical system.
But when perimenopause starts, estrogen levels don't just gently taper off. They go on a wild, unpredictable ride. This hormonal rollercoaster means your heart's conductor is suddenly trying to lead the orchestra through a storm, and things can get a little chaotic.
The Estrogen Effect on Your Heart's Rhythm
The drop in estrogen has a direct impact on your heart. Without its steadying influence, the specialized cells that generate your heart's electrical signals can become more sensitive, or "excitable." This new sensitivity means they might fire off-beat or more forcefully, which you feel as a flutter, a skipped beat, or an intense pounding in your chest.
This isn't just a feeling; it's a well-documented physiological response. If you're in your mid-40s and navigating these changes, you're far from alone. Studies show that up to 42% of perimenopausal women report these unsettling heart palpitations, and that number can climb as high as 54% in postmenopausal women. The hormonal upheaval, particularly plummeting estrogen, directly messes with the cardiovascular system, leading to these very real sensations.
These palpitations aren't just in your head. They are a physical sign that your body is adapting to a new hormonal reality, much like how hormones can affect your mood or sleep.
The Nervous System Connection
Beyond its direct effect on your heart's electrical wiring, estrogen also helps regulate your autonomic nervous system (ANS). The ANS is your body's automatic control center, managing everything from your breathing to your heart rate without you having to think about it. It has two main branches:
- The "Fight or Flight" System (Sympathetic): This is your gas pedal, speeding things up and preparing you for action.
- The "Rest and Digest" System (Parasympathetic): This is your brake, slowing things down to promote calm and recovery.
Estrogen helps keep a nice balance between these two systems. When its levels drop, the "fight or flight" system can start to take over. This means your body might react as if it's under stress even when you're perfectly calm, triggering a sudden adrenaline rush that sends your heart racing. This explains why that heart-pounding sensation can strike out of the blue while you're just reading a book or watching TV.
This shift in your nervous system balance is a key reason why palpitations often feel linked to anxiety. But it's crucial to remember that the hormonal change is often the root cause, not the other way around.
The link between hormones and heart rhythm isn't unique to menopause. Many women notice heart rate changes at different points in their menstrual cycle. For anyone curious about this broader connection, our article on heart palpitations and your period offers more context on how hormonal swings can affect your heart at any stage of life. Understanding this pattern helps reinforce that what you're feeling is a normal part of a major biological transition.
When to Be Concerned About a Pounding Heart
That sudden, forceful pounding in your chest can be unnerving. Your first thought is probably, "Is this dangerous?" It's the right question to ask, and you deserve a clear, calm answer.
While most instances of a menopause heart pounding are simply your body adjusting to new hormonal signals, it's vital to know how to spot the difference between a benign flutter and a real red flag.
The goal here isn't to cause alarm but to empower you with knowledge. When you understand the signs that truly need attention, you can handle the more common, harmless palpitations with a lot more peace of mind. You know your body best, and knowing what to watch for helps you advocate for your health with confidence.
Red Flag Symptoms That Need Attention
Most palpitations are fleeting and harmless, often lasting just a few seconds. However, if that heart-pounding sensation shows up with other specific symptoms, it’s time to seek medical attention. These are the signals that your body might be trying to tell you something more serious is going on than just hormonal shifts.
Pay close attention if your palpitations are accompanied by any of the following:
- Fainting or Feeling Like You Will Faint: A sudden loss of consciousness or feeling extremely lightheaded during an episode is a major red flag.
- Severe Chest Pain: This isn't just a mild ache. We’re talking about significant discomfort, pressure, or pain, especially if it radiates to your arm, jaw, or back.
- Significant Shortness of Breath: Feeling winded after climbing stairs is one thing; struggling to catch your breath while at rest during a palpitation is another.
- Persistent Dizziness or Confusion: Feeling unsteady on your feet or mentally foggy along with a racing heart warrants a professional evaluation.
Understanding Atrial Fibrillation (AFib)
While most palpitations are harmless, menopause is a time when the risk for certain heart rhythm disorders, known as arrhythmias, can increase. One of the most important ones to be aware of is atrial fibrillation, or AFib.
In simple terms, AFib is when the heart's upper chambers (the atria) beat chaotically and irregularly, completely out of sync with the lower chambers. Instead of a strong, steady rhythm, the heart just quivers. This can feel like a fluttering or a rapid, irregular pounding.
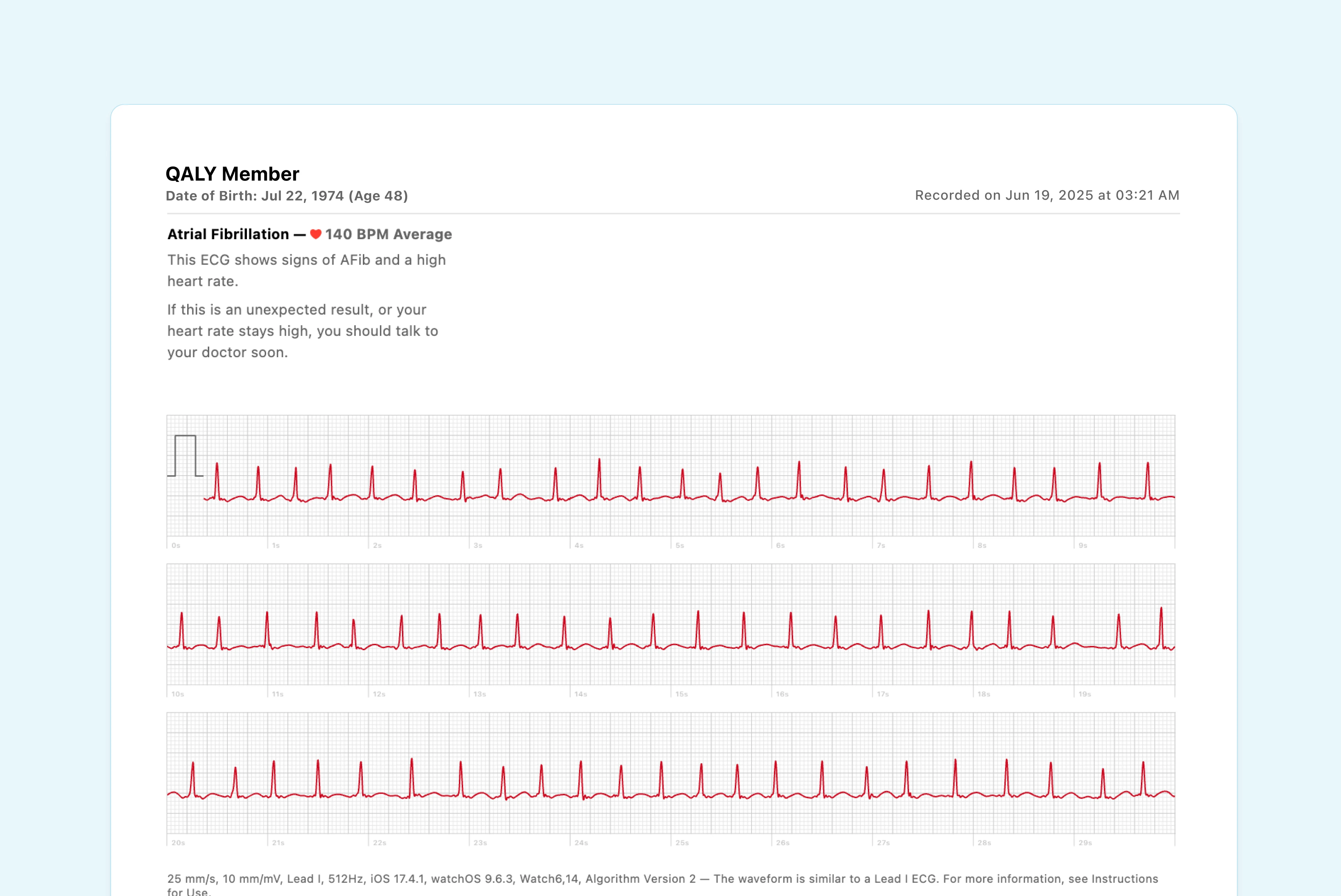
The main concern with AFib is that it can increase the risk of stroke, so identifying it is crucial because it requires a completely different management approach than benign palpitations.
The crucial takeaway is this: A pounding heart alone is usually not an emergency. A pounding heart combined with fainting, severe chest pain, or significant breathing trouble is your cue to get help right away.
It can also be helpful to know that healthcare providers use structured frameworks to make decisions. For instance, many medical approaches are guided by clinical practice guidelines that outline best practices for conditions like heart rhythm disorders. Knowing this helps you understand the methodical approach your doctor will likely take. By recognizing these red flags, you can stay vigilant and make informed decisions about when it's time to seek care.
How to Get Clear Answers from Your Doctor
There's nothing more frustrating than walking into a doctor's office with a real concern, only to feel unheard or dismissed. This is especially true when your symptoms, like a pounding heart, are sporadic and never seem to show up during that quick 15-minute appointment. It's a common story, and it can leave you feeling powerless.
The best way to change this dynamic is to shift the conversation from describing a feeling to presenting cold, hard data. When you can show your doctor exactly what your heart was doing during an episode, the symptom becomes impossible to ignore. This is how you take back control.

Capturing the Evidence at Home
Your menopause heart pounding episodes don't care about your doctor's schedule. They happen when you’re trying to sleep, sitting at your desk, or running errands. The good news is that modern technology means you can finally capture these moments as they happen.
Wearable devices with ECG capabilities, like an Apple Watch, Fitbit, or Kardia, are absolute game-changers here. Instead of just saying, "My heart was racing last Tuesday night," you can record an actual ECG strip of the event. This recording is the single most powerful tool for advocating for yourself, giving your doctor concrete evidence of your heart's rhythm in that exact moment.
This is incredibly important for women in midlife. One pilot study found that 50% of women (ages 46-62) with palpitations experienced them frequently, often daily or at night, sometimes with bursts of atrial tachycardia. The problem? These events were often missed in traditional clinical settings.
Turning Raw Data into Clear Insights
An ECG from your watch is a fantastic start, but let's be honest, it looks like a confusing squiggle to most of us. This is where a service like Qaly becomes so valuable. Instead of trying to guess what the reading means, you can have it analyzed by a certified cardiographic technician in minutes, any time of day or night.
An expert-reviewed report transforms your at-home ECG from a simple recording into a clinical-grade document. It’s something you can hand your doctor with confidence, providing professional context that commands attention.
This report doesn't just identify the rhythm; it provides the crucial metrics a doctor needs to make a real diagnosis. Key details include:
- PR Interval: This measures the time it takes for the electrical signal to get from the top of your heart to the bottom.
- QRS Interval: This shows how long it takes for your heart's lower chambers (the ventricles) to activate or "squeeze."
- QTc Interval: A critical measurement for assessing your risk for certain types of dangerous arrhythmias.
When you walk into your appointment armed with a report detailing these specific intervals and identifying a particular rhythm, the entire conversation changes. You're no longer just describing a vague symptom; you're a proactive partner in your care, presenting tangible data that demands a professional response.
Practical Ways to Manage and Reduce Palpitations
Gaining a sense of control over a pounding heart often starts with small, intentional lifestyle adjustments. While you can't stop hormonal fluctuations, you can manage the triggers that make your heart more sensitive to them.
These strategies aren't about a complete life overhaul. Instead, think of them as gentle ways to support your nervous system and heart, helping them navigate this transition more smoothly.
Identify and Manage Your Triggers
Certain substances can make your heart more "excitable," increasing the likelihood of palpitations. Being mindful of these common culprits is a powerful first step.
Many women find their sensitivity to caffeine skyrockets during menopause. That morning coffee that once felt essential might now be the very thing setting off a racing heart. The same goes for alcohol, which can interfere with your heart's electrical signals.
Consider these small but impactful changes:
- Reduce Stimulants: Try cutting back on caffeine from coffee, tea, and soda. You could switch to decaf or half-caff to see if it makes a difference. Nicotine is another major stimulant that can directly trigger palpitations.
- Limit Alcohol: Pay attention to how your body responds to alcohol. Even one drink can be enough to cause a pounding heart for some, so moderating your intake is key.
Calm Your Nervous System in the Moment
When your heart starts pounding, it can trigger an anxiety response, which in turn makes your heart beat even faster. Breaking this cycle is crucial, and simple breathing techniques can work wonders.
Deep, slow breathing activates your "rest and digest" nervous system, acting like a natural brake on a racing heart. It sends a signal to your brain that you are safe, helping to calm the storm.
One of the most effective methods is box breathing. Inhale slowly for four counts, hold your breath for four counts, exhale for four counts, and hold again for four counts. Repeating this simple pattern can bring immediate relief.
This technique helps regulate your heart rate and gives you a tangible action to focus on when you feel overwhelmed. It’s a tool you can use anywhere, anytime, to regain a sense of calm.
Support Your Body with Hydration and Nutrients
Proper hydration and electrolyte balance are fundamental for a steady heartbeat. Your heart's electrical system relies on minerals like magnesium and potassium to function correctly.
Dehydration can concentrate these electrolytes and put stress on your heart, making palpitations more likely. Aim to drink plenty of water throughout the day.
Many women also find that ensuring they get enough magnesium and potassium through their diet helps. Leafy greens, nuts, seeds, and bananas are excellent sources.
While lifestyle changes are powerful, you can find more in-depth strategies in our guide on how to stop heart palpitations with top relief tips.
Common Questions About Menopause and Your Heart
Even with a better understanding of what's happening in your body, it's completely normal to have lingering questions about these strange new heart sensations. Let's tackle some of the most common concerns we hear from women navigating this phase of life.
Think of this as your go-to guide for a bit of reassurance and clarity. The goal is to help you feel more confident and less anxious about what you're experiencing.
Can Menopause Really Cause My Heart to Pound Like This?
Yes, absolutely. Shifting hormones are one of the biggest culprits behind heart palpitations during perimenopause and menopause. As estrogen levels decline, it can mess with your autonomic nervous system and make your heart's electrical wiring a bit more sensitive. This often leads to that unnerving feeling of a pounding, racing, or skipping heart.
This isn't just in your head; it's a very real physiological response to hormonal changes. In fact, some studies show that up to 54% of postmenopausal women report dealing with palpitations. You are definitely not alone.
Are These Heart Palpitations Dangerous?
For the vast majority of women, these palpitations are benign. That's the medical way of saying they're harmless. They are uncomfortable and scary, for sure, but not a sign of a dangerous heart problem. They're usually just a temporary symptom as your body finds its new normal.
But, and this is important, context matters. If that pounding sensation is ever joined by other symptoms like fainting, severe chest pain, or struggling to catch your breath, that's your cue to seek immediate medical attention.
The key is to distinguish between the sensation itself and other warning signs. A pounding heart on its own is typically not an emergency, but when paired with other severe symptoms, it warrants a professional evaluation.
Will This Feeling Ever Go Away?
This is a question we hear all the time, and it's completely understandable. The good news is that for many women, these palpitations do ease up and eventually fade away as their bodies fully adjust to postmenopause and hormone levels stabilize for good.
Of course, everyone's timeline is different. In the meantime, simple lifestyle shifts can make a huge difference. Things like managing stress, cutting back on caffeine, and staying well-hydrated can often reduce how often they happen and how intense they feel, giving you back a sense of control.
How Can I Be Sure It Isn't Something More Serious?
The only way to know for certain is to get a proper medical evaluation, especially if you have other risk factors for heart disease like high blood pressure or a family history of heart problems. The absolute best way to get answers is to capture what your heart is doing while it's happening.
This is where a wearable device like a smartwatch becomes so valuable. Recording an ECG during an episode gives your doctor real, concrete data to look at. It transforms a vague complaint of "my heart feels funny" into actionable information, leading to an accurate diagnosis and giving you true peace of mind. Your experience is real, and having the data to back it up ensures you're taken seriously.
For a deeper look into what your heart is doing during those unsettling moments, Qaly provides expert, human-reviewed analysis of your smartwatch ECGs in minutes.










.png)
.png)