Key Takeaways
Hello, Heart Hero. Seeing a term like ST segment depression on an ECG from your watch can feel confusing and even a little scary. Let's clear something up right away: it's a signal from your heart's electrical system that deserves attention, but it doesn't automatically mean something is seriously wrong.
Our goal here is to replace that worry with understanding, so you can feel confident about what your body is telling you.
Your Guide to ST Segment Depression
We get it. You’re being proactive about your health, using your watch to stay informed, and then a technical term pops up that sends you down a rabbit hole of internet searches. You're trying to find clear answers, and you've come to the right place. This guide is here to walk you through it with clarity.
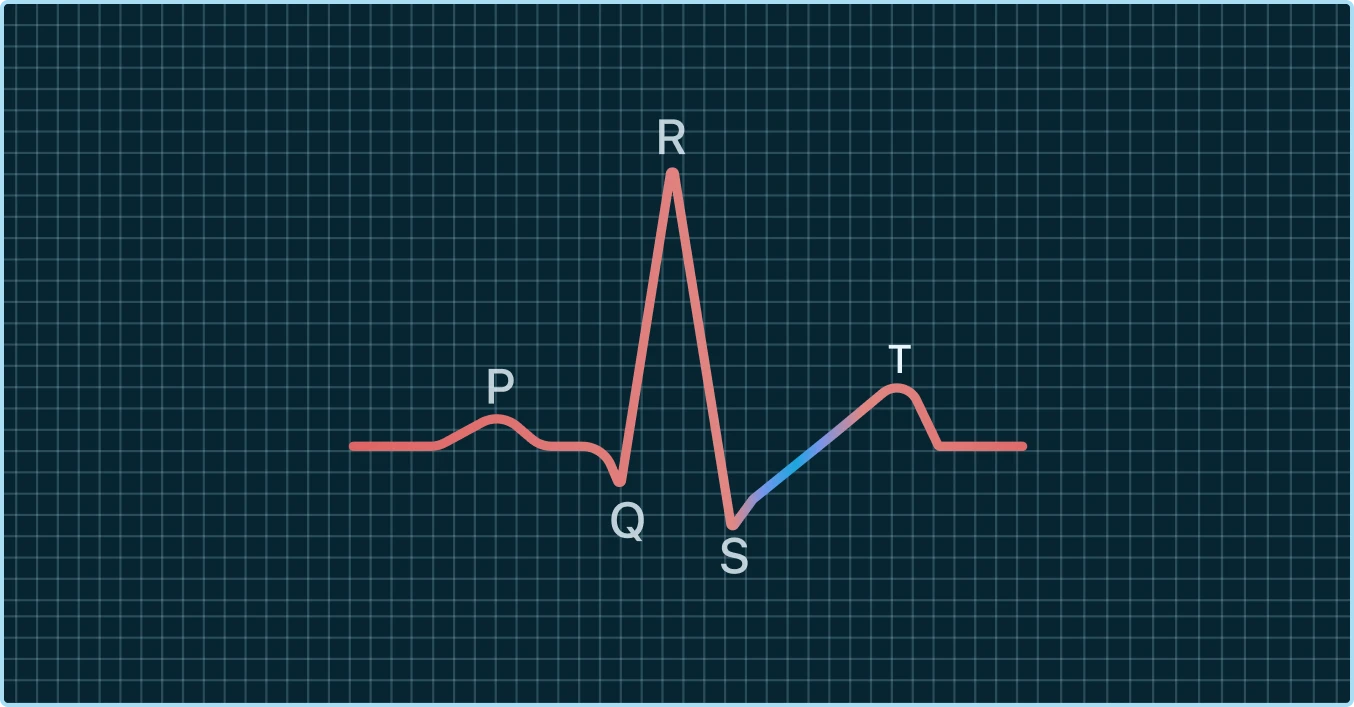
Think of your electrocardiogram (ECG) as a visual story of your heart's electrical journey during a single beat. This story has peaks and valleys, a lot like a wave.
Decoding the ECG Wave
The ST segment is one specific part of this wave. It’s the flat, quiet stretch of the line that comes right after the main, sharp spike (that's the QRS complex). This segment represents a brief resting period for your heart’s main pumping chambers right after they’ve squeezed blood out to the rest of your body.
When you see the word "depression," it simply means this part of the line has dipped below the normal, flat baseline. It’s a visual description, not an emotional one.
Key Takeaway: ST segment depression means the flat part of your heart's electrical wave which represents a recovery phase is lower than it should be. It's a signal, not a diagnosis.
Why This Signal Matters
So, what does this dip mean? It's a sign that something is affecting how your heart muscle cells are "recharging" after a contraction. While it can be associated with reduced blood flow to the heart muscle (ischemia), there are many other potential causes that have nothing to do with blocked arteries.
Understanding this signal is the first step, and you're already doing the right thing by seeking to learn more. This guide will help you understand:
- What ST segment depression actually means for your heart.
- Why the specific shape and measurement of the dip are so important.
- How your smartwatch ECG is different from a 12-lead ECG you'd get at a hospital.
- What practical steps you should take if you see this on your watch.
Being proactive with your health means being informed. While your wearable provides valuable data, knowing its limitations and context is crucial. For a deeper dive into making sense of these readings, check out our cardiologist's guide to the smartwatch ECG. It’s all about empowering you to take the right next steps on your heart health journey.
What ST Segment Depression Actually Means
To really get what ST segment depression is, let's peek inside your heart. Think of each heart muscle cell as a tiny, rechargeable battery. After every single heartbeat, these little batteries have to reset and recharge for the next beat.
That critical recharging phase is exactly what the ST segment on your ECG shows. Ideally, it should be a calm, flat line. A "depression" simply means something has messed with this recharging process, causing that line to dip downwards. This dip is a visual cue that your heart muscle might be under some kind of stress.
Two Main Buckets of Causes
When a doctor spots ST segment depression, their mind usually sorts the potential causes into two big categories. Knowing these can take you from feeling confused to having a clear picture of why your watch is showing you this.
The first and most talked-about category has to do with blood flow. The medical term for this is ischemia (pronounced is-kee-mia).
Picture your heart muscle like a car engine trying to power up a steep hill. The harder it works, the more fuel it needs in this case, oxygen-rich blood. Ischemia is a classic supply-and-demand problem: the heart muscle is demanding more oxygen than the coronary arteries can deliver at that moment.
This imbalance can happen for a couple of reasons:
- A blockage: Plaque buildup in the arteries can create a traffic jam for blood flow.
- Increased demand: During exercise or high stress, your heart ramps up, beating faster and harder, which requires way more oxygen.
When the heart muscle is starved for oxygen, even for a short time, it can throw off that cellular recharging process. The result? The dip we see as ST segment depression. This is precisely why healthcare professionals pay close attention to it, as it can be a clue to underlying coronary artery disease.
Beyond Blocked Arteries
But here’s a crucial point that often gets lost in panicked late-night Googling: ischemia isn't the only cause. This misunderstanding creates a ton of unnecessary anxiety for people using wearable ECGs. Many other things can cause ST segment depression, and they all fall into a second, much broader bucket of non-ischemic causes.
These are situations where the heart's blood supply is perfectly fine, but something else is interfering with the heart’s electrical system and its ability to recharge properly.
Important Insight: A dip in your ST segment does not automatically mean you have a blocked artery. Many factors unrelated to blood flow can cause this ECG finding, which is why context and professional review are so vital.
Here are some common non-ischemic culprits:
- A Very Fast Heart Rate: When your heart is racing (tachycardia), the cells just don't get enough time to fully recharge between beats. This can create a temporary and often harmless ST depression that disappears once your heart rate comes back down.
- Certain Medications: Some common drugs, including certain heart rhythm medications or even some antibiotics, can alter the electrical properties of your heart cells and lead to ST segment changes.
- Electrolyte Imbalances: Your heart’s electrical wiring depends on a precise balance of minerals like potassium and magnesium. If these levels are out of whack, it can disrupt the recharging phase.
- Structural Heart Changes: Conditions like an enlarged heart muscle (left ventricular hypertrophy) can change the ECG’s overall appearance and cause ST segment depression, even with no blockages in sight.
Getting a handle on what an ECG actually shows is a huge first step in making sense of these signals from your body. To take it further, you can explore our detailed guide on how to read an ECG. The more you know about the basics, the better the conversations you can have with your doctor.
Why the Shape of the Dip Matters
When you look at an ECG, it’s tempting to think that a dip is just a dip. But in the world of cardiology, not all instances of ST segment depression are created equal. The specific shape, or morphology, of that dip provides crucial clues that help experts understand what might be happening with your heart.
Think of it like a detective looking at footprints in the sand. A deep, sharp print tells a different story than a shallow, scuffed one. It's the same idea here; the contour of the ST segment tells a unique story about your heart's electrical activity.
Let's break down the three main patterns you might hear about, using some simple analogies to make them clear.
The Three Key Shapes of ST Segment Depression
When interpreting an ECG, cardiologists look for distinct patterns in how the ST segment deviates from the flat baseline.
- Upsloping ST Depression: Imagine a ski ramp that gently slopes back uphill. This is what an upsloping pattern looks like. The ST segment dips down but immediately starts to climb back toward the baseline. This shape is often, but not always, considered less concerning, especially when it pops up during a fast heart rate.
- Horizontal ST Depression: Picture a perfectly flat, level shelf that is simply lower than the main countertop. This is a horizontal pattern. The ST segment drops and runs parallel to the baseline for a bit before rising again. This shape is generally considered more significant than an upsloping one.
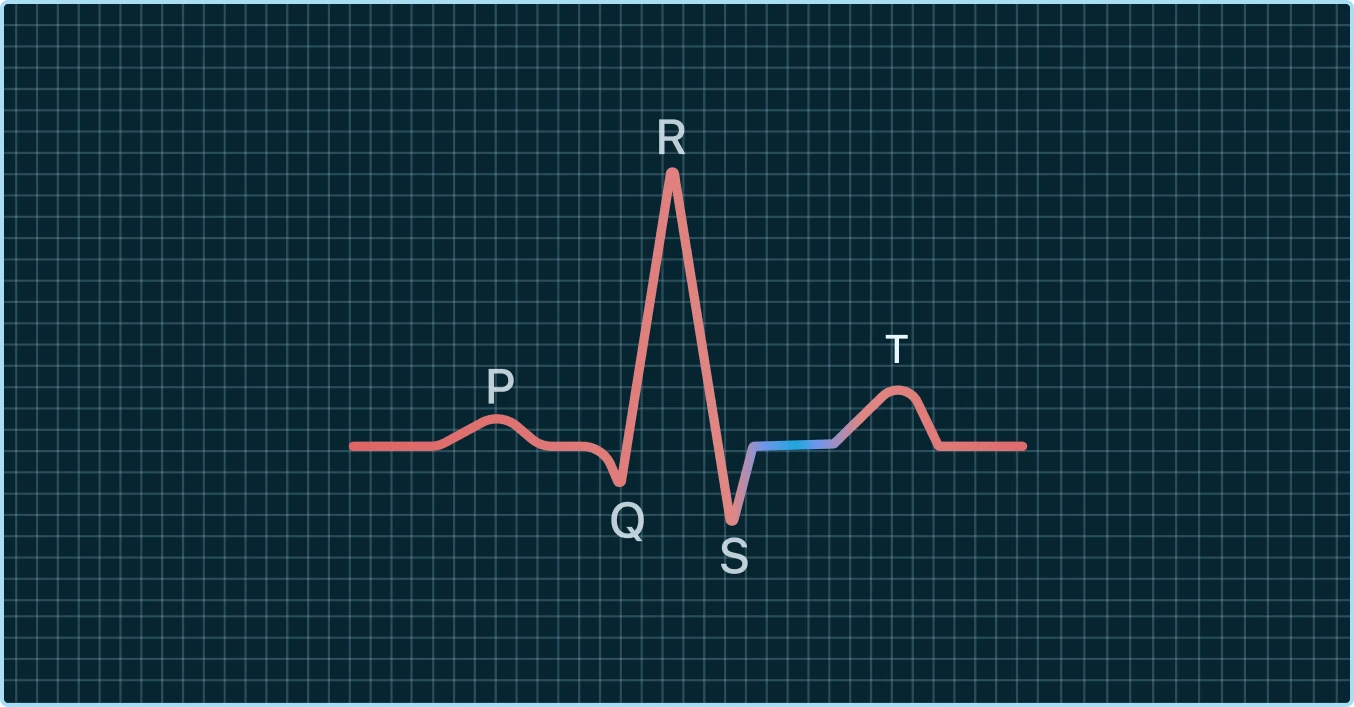
- Downsloping ST Depression: Think of a slide at a playground. A downsloping pattern shows the ST segment dipping and continuing on a downward trajectory. Along with the horizontal pattern, downsloping ST segment depression is often viewed as a more clinically important sign that warrants a closer look.
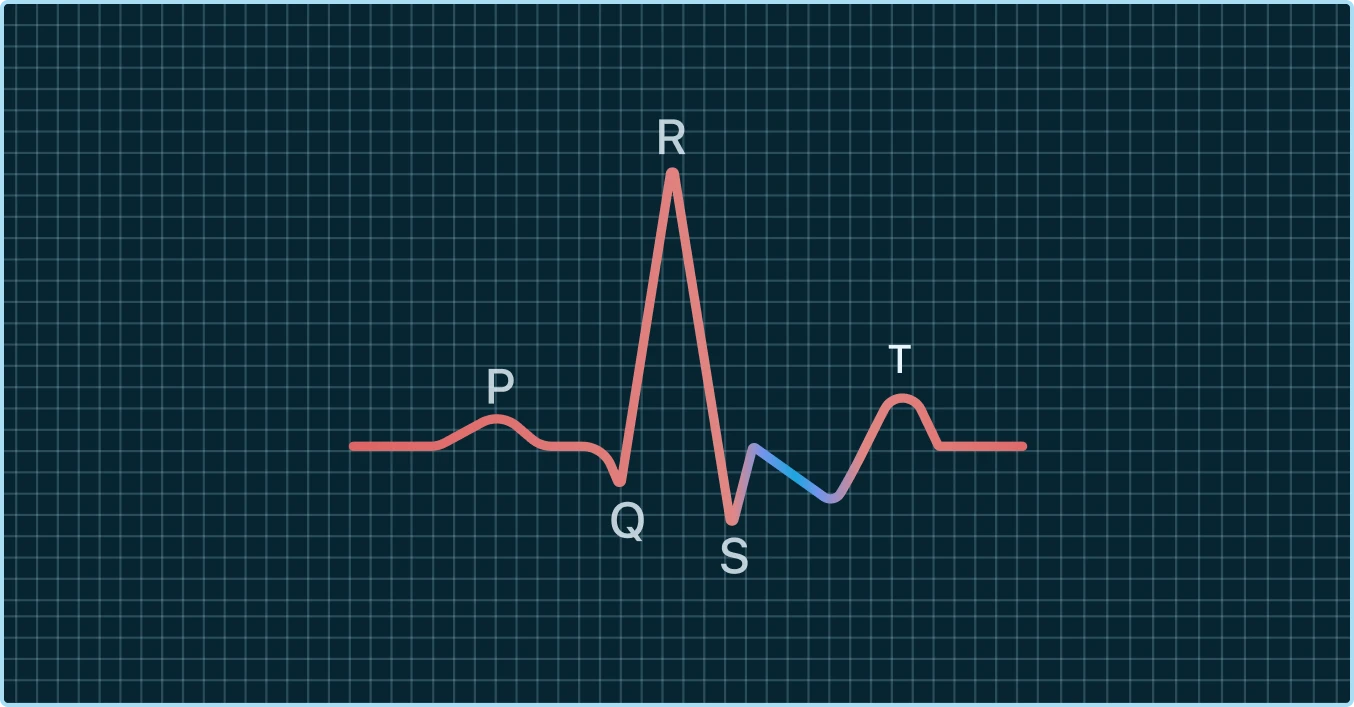
How Deep Does It Go?
Besides the shape, the depth of the dip also matters. You might see measurements like "0.5 mm" or "1 mm" of depression. On an ECG grid, millimeters measure the vertical drop from the baseline. A deeper depression is generally more significant.
For instance, a depression of 0.5 mm or more in two related leads is a common threshold that technicians and doctors look for as a potentially meaningful finding.
Key Insight: Both the shape (upsloping, horizontal, or downsloping) and the depth (measured in mm) of ST segment depression are critical pieces of the puzzle. A horizontal or downsloping dip is typically considered more concerning than an upsloping one.
It's important to understand that these are general guidelines. For years, the upsloping pattern was often dismissed as a "false positive," especially during exercise tests. However, emerging research reminds us that context is everything.
One study looking at patients with suspected coronary artery disease found that while upsloping ST depression was rare, every single patient who showed that isolated pattern was later found to have significant blockages. This challenges old assumptions and highlights why a blanket rule can be risky. You can read more about these interesting findings.
This complexity is exactly why getting an expert review of any ST segment depression you see on your watch is so valuable. A trained eye can analyze the shape, depth, and your heart rate to interpret the signal correctly, giving you clarity instead of leaving you to guess.
How Your Watch ECG Compares to a Hospital ECG
Getting acquainted with the device on your wrist can significantly benefit your heart health. Think of your watch as an excellent screening tool, not a comprehensive diagnostic device.
Consider this analogy: Your watch provides a single-lead ECG, akin to capturing a single, well-framed photograph of your heart's electrical activity from one specific angle. This snapshot is useful for identifying certain rhythm issues. In contrast, a 12-lead ECG in a hospital or doctor's office is like recording a complete, 360-degree, high-definition video of the same activity. By placing ten electrodes on your chest, arms, and legs, it captures twelve different electrical perspectives simultaneously, offering doctors a detailed, multi-dimensional view to detect problems that may be invisible from a single angle.
Can you see ST segment changes on your smartwatch? Sometimes, yes - but here's why you shouldn't rely solely on it: Smartwatch ECGs can occasionally detect ST segment changes, but they are often obscured by background noise or resemble motion artifacts (such as wrist movements). Since smartwatches only capture one lead from your wrist, they lack the comprehensive view needed by doctors. The thing about ST changes is that even when they appear clearly, they require context.
Why More Views Matter
The difference between a single snapshot and a complete video is huge, especially for something as complex as ST segment depression. A 12-lead ECG can confirm if what your watch saw is real, pinpoint its location on the heart muscle, and give a much clearer idea of what might be causing it.
This is exactly why your watch is such a powerful first-alert system but can't take the place of a full clinical workup. It’s designed to flag potential issues so you can start a more informed conversation with your doctor.
When we talk about reliability, we often get into understanding diagnostic accuracy metrics like sensitivity and specificity. These concepts are key to understanding why the 12-lead ECG remains the gold standard for making a definitive diagnosis.
The Challenge of "Noise"
Another really important factor is something called "noise"; basically, any electrical interference that messes with your watch’s reading. Since your watch ECG relies on just two points of contact (your wrist and your fingertip), it can be sensitive to things that distort the signal.
Common culprits for noise include:
- Movement: Even slight twitches in your arm or body can create a shaky, unreadable ECG tracing.
- Poor Contact: If your skin is too dry or you aren’t pressing firmly enough on the watch crown, you can get a weak signal.
- Electrical Interference: Other electronics buzzing nearby can sometimes interfere with the recording.
This noise can sometimes look like real heart rhythm changes or even mimic ST segment depression, causing a lot of unnecessary worry. A hospital ECG gets around this by using sticky electrodes and having you lie perfectly still.
Your Watch as a Health Journal: It's helpful to think of your watch as a personal health journal, not a diagnostic lab. It captures moments and gives you clues. The data is incredibly valuable, but it’s the beginning of an investigation, not the final word.
Knowing these limitations doesn't make your device any less powerful. In fact, it helps you use it smarter. The key is knowing how to get a clean reading and when it’s time to call in a professional. For a deeper dive into what your watch can and can't do, check out our article on how accurate the ECG is on your Apple Watch.
What to Do When You See ST Segment Depression
Seeing an alert for ST segment depression on your watch ECG can make your own heart skip a beat. It's an unsettling moment, for sure. But your next steps can be calm, clear, and methodical.
The most important thing to do first is simple: don’t panic. An isolated reading can be thrown off by all sorts of things, like movement or a poor connection between your skin and the watch. Your first move should be to gather more information, not jump to the worst conclusion.
Take a Better Reading
Before you do anything else, try to capture the cleanest ECG signal you can. Think of it like taking a photo in low light; you have to stay perfectly still to avoid a blurry picture.
- Sit down and relax. Find a quiet spot where you can sit undisturbed for a minute or two.
- Rest your arm. Place the arm with your watch on a flat, stable surface like a table or your lap. This helps minimize the tiny muscle tremors that create "noise" in your ECG.
- Breathe deep. Take a few slow, deep breaths to let your heart rate settle. A calm body helps produce a cleaner signal.
- Take a new ECG. Start a new reading, making sure you keep good, firm contact with the sensor the whole time.
Often, a second, cleaner reading will come back looking completely normal. But if that ST segment depression shows up again, your next step is to listen carefully to your body.

Pay Attention to Your Symptoms
Your ECG is just one piece of the puzzle. How you physically feel provides the most critical context. Seeing ST segment depression alongside certain symptoms changes the situation from "something to watch" to "something that needs immediate medical attention."
You should seek emergency care right away if your ECG shows ST depression and you experience any of these symptoms:
- Chest pain, pressure, squeezing, or a feeling of fullness
- Shortness of breath or finding it hard to breathe
- Dizziness, lightheadedness, or feeling like you might faint
- Pain or discomfort that spreads to your jaw, neck, back, or down one or both arms
- Breaking out in a cold sweat or having clammy skin
These are the classic signs of a potential heart attack. In a hospital, doctors would quickly run blood tests to check for specific cardiac enzymes that signal heart muscle damage. You can learn more about key indicators like troponin levels to understand how they help diagnose these events.
Sharing Your ECG with a Professional
So, what if you see ST segment depression but feel perfectly fine? This is where being proactive is your best tool. The goal is to get your ECG in front of a trained professional who can tell you what it really means.
Crucial Reminder: A single-lead ECG from your watch is a screening tool, not a diagnostic one. It can't see the full 3D picture of your heart's electricity like a 12-lead hospital ECG, but it provides incredibly valuable clues that can kickstart a necessary conversation with your doctor.
For those of us using home and wearable ECGs, this means that even subtle horizontal or downsloping ST depression of 0.5–1.0 mm, especially if it comes with chest discomfort or shortness of breath, can point to the same serious issues that fill emergency rooms every day. It might not look as dramatic as a full-blown STEMI on an ECG strip, but it warrants a professional look.
Here’s how you can share your data effectively:
- Save the ECG as a PDF. Use your device’s app to save the reading. A PDF is the best format because it’s easy to share and preserves the entire waveform clearly.
- Send it to your doctor. Most doctors have a patient portal where you can securely send messages and attachments. Email the PDF to your primary care physician or cardiologist with a quick note about when you took it and if you felt any symptoms.
- Use an interpretation service. For a fast, expert review, you can upload your ECG directly to an app like Qaly. A certified technician will analyze it and send you a clear report, often in minutes, giving you peace of mind or confirming that you need to follow up with your doctor.
When facing potential health concerns like ST segment depression, knowing what resources are available, can help you get timely care. By taking these methodical steps, you shift from being a passive worrier to an empowered, active partner in your own health journey.
Get Clarity and Peace of Mind with Qaly
Trying to navigate the healthcare system can feel like an uphill battle. It's frustrating, especially when you have data from your watch showing something concerning, but getting a timely, clear answer feels impossible.
You can wait weeks for a doctor's appointment, only to feel rushed or unheard when you finally get there. This gap between the data on your wrist and a professional’s insight is exactly why Qaly was created. We knew there had to be a better way.
Your Personal Heart Health Ally
Instead of waiting and worrying, Qaly gives you direct access to expert analysis of your ECGs. We connect you with certified cardiographic technicians who are available 24/7 to review your readings, with no appointment needed.
With Qaly, you get a clear, human-written report analyzing your ECG in just minutes. It’s about replacing uncertainty and anxiety with knowledge and confidence so you can take charge of your heart health.
This rapid feedback is a powerful tool. It helps you understand whether a strange reading was just "noise" from movement or something that truly warrants a follow-up conversation with your doctor.
More Than Just a Single Reading
Your heart health is a journey, not just a single snapshot in time. Qaly is designed to be your partner on that journey by helping you track your ECG readings over time. Every analysis is saved, creating a valuable, organized record of your heart’s activity.
This historical data is incredibly useful for a few key reasons:
- Spotting Trends: You can see if it is a one-off thing or part of a developing pattern.
- Identifying Triggers: By tracking readings, you might start to see connections between your ECG and your lifestyle, like stress or physical exertion.
- Informing Doctor Visits: You can walk into your appointments with a comprehensive report, ready to show your doctor exactly what you've been seeing.
This turns a potentially stressful doctor’s visit into a more productive and meaningful conversation. You’re no longer just trying to describe a feeling; you’re presenting clear, organized data that your care team can act on.
Ultimately, Qaly provides more than just data. It’s a tool that offers confidence, reassurance, and a proactive way to manage your well-being. By giving you immediate access to professional analysis, Qaly helps you understand your body better and become a true advocate for your own heart health.
Common Questions About ST Depression on Your Watch
Seeing ST depression on your watch can bring up a lot of questions. Let's tackle some of the most common ones.
Can Anxiety or Stress Cause ST Segment Depression?
It’s possible, yes. A heart that’s beating very quickly during a moment of intense anxiety or a panic attack can sometimes show what’s called rate-related ST depression. This typically has an upsloping shape and tends to go away as your heart rate slows back down.
But here’s the thing: you can’t reliably figure out if it’s from anxiety or something more serious just by looking at it yourself. If you see ST depression during a high-stress moment, especially if you’re also feeling chest tightness, the safest move is to get it professionally reviewed.
Should I Exercise to Trigger ST Segment Depression?
Absolutely not. You should never, ever try to perform your own "stress test" at home. While it's true that exercise can bring out ST segment depression related to coronary artery disease, trying to force this to happen without medical supervision is incredibly dangerous.
If you’re worried about how your heart handles physical activity, talk to your doctor. Share your concerns and any ECGs you’ve managed to capture. They are the only ones who can decide if you need a formal, medically supervised stress test in a clinical setting.
Important Safety Note: A medical stress test is done in a controlled environment with emergency equipment on standby for a reason. Attempting to replicate this on your own carries a significant risk to your safety.
What Are Nonspecific ST-T Wave Changes?
You might see the term "nonspecific" on an ECG report. This is what we use when your ECG shows minor changes in the ST segment or T wave that don't fit the classic pattern for any specific condition. It simply means a small deviation was seen, but it isn't distinct enough on its own to point to a definite problem.
These subtle changes can be triggered by a lot of things, from medications to normal variations between people. While they are often harmless, tracking them over time is smart. It helps your doctor see if a more specific pattern ever develops, which can be valuable information.
Trying to make sense of these complex heart signals on your own is tough, but getting clear answers shouldn't be. Qaly provides expert, human-reviewed analysis of your smartwatch ECGs in minutes.










.png)
.png)